Applications of data envelopment analysis in acute care hospitals: a systematic literature review, 1984–2022
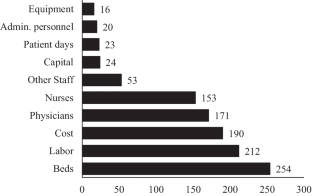
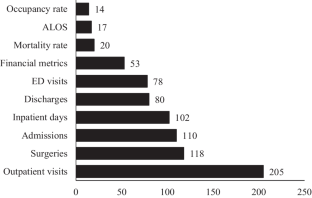
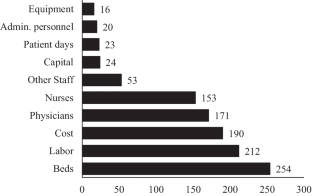
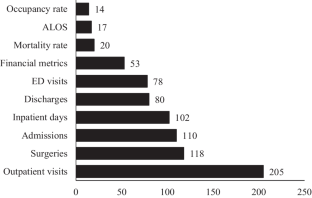
This study reviews scholarly publications on data envelopment analysis (DEA) studies on acute care hospital (ACH) efficiency published between 1984 and 2022 in scholarly peer-reviewed journals. We employ systematic literature review (SLR) method to identify and analyze pertinent past research using predetermined steps. The SLR offers a comprehensive resource that meticulously analyzes DEA methodology for practitioners and researchers focusing on ACH efficiency measurement. The articles reviewed in the SLR are analyzed and synthesized based on the nature of the DEA modelling process and the key findings from the DEA models. The key findings from the DEA models are presented under the following sections: effects of different ownership structures; impacts of specific healthcare reforms or other policy interventions; international and multi-state comparisons; effects of changes in competitive environment; impacts of new technology implementations; effects of hospital location; impacts of quality management interventions; impact of COVID-19 on hospital performance; impact of teaching status, and impact of merger. Furthermore, the nature of DEA modelling process focuses on use of sensitivity analysis; choice of inputs and outputs; comparison with Stochastic Frontier Analysis; use of congestion analysis; use of bootstrapping; imposition of weight restrictions; use of DEA window analysis; and exogenous factors. The findings demonstrate that, despite several innovative DEA extensions and hospital applications, over half of the research used the conventional DEA models. The findings also show that the most often used inputs in the DEA models were labor-oriented inputs and hospital beds, whereas the most frequently used outputs were outpatient visits, followed by surgeries, admissions, and inpatient days. Further research on the impact of healthcare reforms and health information technology (HIT) on hospital performance is required, given the number of reforms being implemented in many countries and the role HIT plays in enhancing care quality and lowering costs. We conclude by offering several new research directions for future studies.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save
Springer+ Basic
€32.70 /Month
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Buy Now
Price includes VAT (France)
Instant access to the full article PDF.
Rent this article via DeepDyve

Similar content being viewed by others
The use of Data Envelopment Analysis (DEA) in healthcare with a focus on hospitals
Article 24 February 2018

Data Envelopment Analysis and Malmquist Index Application: Efficiency of Hospitals Networks in Morocco
Chapter © 2024
Primary Care Efficiency Measurement Using Data Envelopment Analysis: A Systematic Review
Article 26 November 2014
Explore related subjects
Data availability
Data sources are properly cited. All details for performing our analysis are reported in the manuscript.
References
- OECD (2021) Health at a Glance 2021: OECD Indicators. OECD. https://doi.org/10.1787/ae3016b9-en
- Samuelson K (2017) The role of hospitals in community and economic development. Fels Institute of Government, University of Pennsylvania. https://www.fels.upenn.edu/recap/posts/1071. Accessed 6 Nov 2021
- CMS (2022) National Health Expenditures 2020 Highlights. Baltimore, MD: Centers for Medicare & Medicaid Services
- Chilingerian JA, Sherman HD (2004) Health care applications. In: Cooper WW, Seiford LM, Zhu J (eds). Handbook on Data Envelopment Analysis, vol. 71, Boston: Kluwer Academic Publishers. p 481–537. https://doi.org/10.1007/1-4020-7798-X_17.
- Hollingsworth B (2003) Non-parametric and parametric applications measuring efficiency in health care. Health Care Manag Sci 6:203–218. https://doi.org/10.1023/a:1026255523228ArticleGoogle Scholar
- Hollingsworth B (2008) The measurement of efficiency and productivity of health care delivery. Health Econ 17:1107–1128. https://doi.org/10.1002/hec.1391ArticleGoogle Scholar
- Hollingsworth B, Dawson PJ, Maniadakis N (1999) Efficiency measurement of health care: a review of non-parametric methods and applications. Health Care Manag Sci 2:161–172. https://doi.org/10.1023/a:1019087828488ArticleGoogle Scholar
- Kohl S, Schoenfelder J, Fügener A, Brunner JO (2019) The use of Data Envelopment Analysis (DEA) in healthcare with a focus on hospitals. Health Care Manag Sci 22:245–286. https://doi.org/10.1007/s10729-018-9436-8ArticleGoogle Scholar
- O’Neill L, Rauner M, Heidenberger K, Kraus M (2008) A cross-national comparison and taxonomy of DEA-based hospital efficiency studies. Socioecon Plann Sci 42:158–189. https://doi.org/10.1016/j.seps.2007.03.001ArticleGoogle Scholar
- Tiemann O, Schreyögg J, Busse R (2012) Hospital ownership and efficiency: a review of studies with particular focus on Germany. Health Policy 104:163–171. https://doi.org/10.1016/j.healthpol.2011.11.010ArticleGoogle Scholar
- Giancotti M, Guglielmo A, Mauro M (2017) Efficiency and optimal size of hospitals: Results of a systematic search. PLoS ONE 12:e0174533. https://doi.org/10.1371/journal.pone.0174533ArticleGoogle Scholar
- Kiadaliri AA, Jafari M, Gerdtham U-G (2013) Frontier-based techniques in measuring hospital efficiency in Iran: a systematic review and meta-regression analysis. BMC Health Serv Res 13:312. https://doi.org/10.1186/1472-6963-13-312ArticleGoogle Scholar
- Mahdiyan S, Dehghani A, Tafti AD, Pakdaman M, Askari R (2019) Hospitals’ efficiency in Iran: A systematic review and meta-analysis. J Educ Health Promot 8:126. https://doi.org/10.4103/jehp.jehp_393_18ArticleGoogle Scholar
- Ravaghi H, Afshari M, Isfahani P, Bélorgeot VD (2019) A systematic review on hospital inefficiency in the Eastern Mediterranean Region: sources and solutions. BMC Health Serv Res 19:830. https://doi.org/10.1186/s12913-019-4701-1ArticleGoogle Scholar
- Audibert M, Mathonnat J, Pelissier A, Huang XX, Ma A (2013) Health insurance reform and efficiency of township hospitals in rural China: An analysis from survey data. China Econ Rev 27:326–338. https://doi.org/10.1016/j.chieco.2013.01.004ArticleGoogle Scholar
- Herwartz H, Strumann C (2012) On the effect of prospective payment on local hospital competition in Germany. Health Care Manag Sci 15:48–62. https://doi.org/10.1007/s10729-011-9180-9ArticleGoogle Scholar
- Hu H-H, Qi Q, Yang C-H (2012) Analysis of hospital technical efficiency in China: Effect of health insurance reform. China Econ Rev 23:865–877. https://doi.org/10.1016/j.chieco.2012.04.008ArticleGoogle Scholar
- Tiemann O, Schreyögg J (2009) Effects of Ownership on Hospital Efficiency in Germany. Bus Res 2:115–145. https://doi.org/10.1007/BF03342707ArticleGoogle Scholar
- Assari Arani A, Atashbar T, Antoun J, Bossert T (2018) Iran’s Health Reform Plan: Measuring Changes in Equity Indices. Iran J Public Health 47:390–396 Google Scholar
- Ökem ZG, Çakar M (2015) What have health care reforms achieved in Turkey? An appraisal of the “Health Transformation Programme.” Health Policy 119:1153–1163. https://doi.org/10.1016/j.healthpol.2015.06.003ArticleGoogle Scholar
- Shaw FE, Asomugha CN, Conway PH, Rein AS (2014) The Patient Protection and Affordable Care Act: opportunities for prevention and public health. The Lancet 384:75–82. https://doi.org/10.1016/S0140-6736(14)60259-2ArticleGoogle Scholar
- Shou-Hsia C, Tung-Liang C (1997) The Effect of Universal Health Insurance on Health Care Utilization in Taiwan: Results From a Natural Experiment. JAMA 278:89–93. https://doi.org/10.1001/jama.1997.03550020017009ArticleGoogle Scholar
- Yip W, Fu H, Chen AT, Zhai T, Jian W, Xu R et al (2019) 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. The Lancet 394:1192–1204. https://doi.org/10.1016/S0140-6736(19)32136-1ArticleGoogle Scholar
- Pereira MA, Ferreira DC, Figueira JR, Marques RC (2021) Measuring the efficiency of the Portuguese public hospitals: A value modelled network data envelopment analysis with simulation. Expert Syst Appl 181:115169. https://doi.org/10.1016/j.eswa.2021.115169ArticleGoogle Scholar
- Kao C, Pang R-Z, Liu S-T, Bai X-J (2021) Most productive types of hospitals: An empirical analysis. Omega 99:102310. https://doi.org/10.1016/j.omega.2020.102310ArticleGoogle Scholar
- Lindlbauer I, Winter V, Schreyögg J (2016) Antecedents and Consequences of Corporatization: An Empirical Analysis of German Public Hospitals. J Public Admin Res Theory 26:309–326. https://doi.org/10.1093/jopart/muv016ArticleGoogle Scholar
- Cinaroglu S (2020) Integrated k-means clustering with data envelopment analysis of public hospital efficiency. Health Care Manag Sci 23:325–338. https://doi.org/10.1007/s10729-019-09491-3ArticleGoogle Scholar
- Mitropoulos P, Talias ΜA, Mitropoulos I (2015) Combining stochastic DEA with Bayesian analysis to obtain statistical properties of the efficiency scores: An application to Greek public hospitals. Eur J Oper Res 243:302–311. https://doi.org/10.1016/j.ejor.2014.11.012ArticleGoogle Scholar
- Peyrache A (2013) Industry structural inefficiency and potential gains from mergers and break-ups: A comprehensive approach. Eur J Oper Res 230:422–430. https://doi.org/10.1016/j.ejor.2013.04.034ArticleGoogle Scholar
- Schneider AM, Oppel E-M, Schreyögg J (2020) Investigating the link between medical urgency and hospital efficiency – Insights from the German hospital market. Health Care Manag Sci 23:649–660. https://doi.org/10.1007/s10729-020-09520-6ArticleGoogle Scholar
- Wang BB, Ozcan YA, Wan TT, Harrison J (1999) Trends in hospital efficiency among metropolitan markets. J Med Syst 23:83–97. https://doi.org/10.1023/a:1020585118381ArticleGoogle Scholar
- Adelman D (2020) An Efficient Frontier Approach to Scoring and Ranking Hospital Performance. Oper Res 68:762–792. https://doi.org/10.1287/opre.2019.1972ArticleGoogle Scholar
- Kitchenham B, Charters S (2007) Guidelines for performing systematic literature reviews in software engineering
- Ding DX (2014) The effect of experience, ownership and focus on productive efficiency: A longitudinal study of U.S. hospitals. J Operations Manage 32:1–14. https://doi.org/10.1016/j.jom.2013.10.002.
- Grosskopf S, Valdmanis V (1987) Measuring hospital performance: A non-parametric approach. J Health Econ 6:89–107. https://doi.org/10.1016/0167-6296(87)90001-4ArticleGoogle Scholar
- Burgess JF, Wilson PW (1996) Hospital Ownership and Technical Inefficiency. Manage Sci 42:110–123 ArticleGoogle Scholar
- White KR, Ozcan YA (1996) Church ownership and hospital efficiency. Hosp Health Serv Adm 41:297–310 Google Scholar
- Ozcan YA, Luke RD, Haksever C (1992) Ownership and organizational performance. A comparison of technical efficiency across hospital types. Med Care 30:781–94
- Valdmanis V (1990) Ownership and technical efficiency of hospitals. Med Care 28:552–561. https://doi.org/10.1097/00005650-199006000-00007ArticleGoogle Scholar
- Helmig B, Lapsley I (2001) On the efficiency of public, welfare and private hospitals in Germany over time: a sectoral data envelopment analysis study. Health Serv Manage Res 14:263–274. https://doi.org/10.1258/0951484011912762ArticleGoogle Scholar
- Harrison JP, Sexton C (2006) The improving efficiency frontier of religious not-for-profit hospitals. Hosp Top 84:2–10. https://doi.org/10.3200/HTPS.84.1.2-10ArticleGoogle Scholar
- Roh C-Y, Moon M, Jung K (2013) Efficiency Disparities among Community Hospitals in Tennessee: Do Size, Location, Ownership, and Network Matter? J Health Care Poor Underserved 24:1816–1833. https://doi.org/10.1353/hpu.2013.0175ArticleGoogle Scholar
- Gruca TS, Nath D (2001) The technical efficiency of hospitals under a single payer system: the case of Ontario community hospitals. Health Care Manag Sci 4:91–101. https://doi.org/10.1023/a:1011401510010ArticleGoogle Scholar
- Roh C-Y, Jae Moon M, Jung C (2010) Measuring performance of U.S. nonprofit hospitals. Public Perform Manage Rev 34:22–37. https://doi.org/10.2753/PMR1530-9576340102.
- Lee K-H, Yang S-B, Choi M (2009) The Association between Hospital Ownership and Technical Efficiency in a Managed Care Environment. J Med Syst 33:307–315. https://doi.org/10.1007/s10916-008-9192-2ArticleGoogle Scholar
- Chang H, Cheng M-A, Das S (2004) Hospital ownership and operating efficiency: Evidence from Taiwan. Eur J Oper Res 159:513–527. https://doi.org/10.1016/S0377-2217(03)00412-0ArticleGoogle Scholar
- Czypionka T, Kraus M, Mayer S, Röhrling G (2014) Efficiency, ownership, and financing of hospitals: the case of Austria. Health Care Manag Sci 17:331–347. https://doi.org/10.1007/s10729-013-9256-9ArticleGoogle Scholar
- Shah A, Bishop SM, Ramsay C, Schneider EC (2018) Maryland’s global budget program: Still an option for containing costs. To the Point. New York, NY
- Yan J, Lin H-H, Zhao D, Hu Y, Shao R (2019) China’s new policy for healthcare cost-control based on global budget: a survey of 110 clinicians in hospitals. BMC Health Serv Res 19:84. https://doi.org/10.1186/s12913-019-3921-8ArticleGoogle Scholar
- Borden JP (1988) An assessment of the impact of diagnosis-related group (DRG)-based reimbursement on the technical efficiency of New Jersey hospitals using data envelopment analysis. J Account Public Policy 7:77–96 ArticleGoogle Scholar
- Garcia-Lacalle J, Martin E (2010) Rural vs urban hospital performance in a ‘competitive’ public health service. Soc Sci Med 71:1131–1140. https://doi.org/10.1016/j.socscimed.2010.05.043ArticleGoogle Scholar
- Biørn E, Hagen TP, Iversen T, Magnussen J (2003) The Effect of Activity-Based Financing on Hospital Efficiency: A Panel Data Analysis of DEA Efficiency Scores 1992–2000. Health Care Manag Sci 6:271–283. https://doi.org/10.1023/A:1026212820367ArticleGoogle Scholar
- Maniadakis N, Hollingsworth B, Thanassoulis E (1999) The impact of the internal market on hospital efficiency, productivity and service quality. Health Care Manag Sci 2:75–85. https://doi.org/10.1023/a:1019079526671ArticleGoogle Scholar
- Mollahaliloglu S, Kavuncubasi S, Yilmaz F, Younis MZ, Simsek F, Kostak M et al (2018) Impact of health sector reforms on hospital productivity in Turkey: Malmquist index approach. Intl J Organ Theory Behav 21:72–84. https://doi.org/10.1108/IJOTB-03-2018-0025ArticleGoogle Scholar
- Sulku SN (2012) The health sector reforms and the efficiency of public hospitals in Turkey: provincial markets. Eur J Public Health 22:634–638. https://doi.org/10.1093/eurpub/ckr163ArticleGoogle Scholar
- Polyzos N (2012) A three-year Performance Evaluation of the NHS Hospitals in Greece. Hippokratia 16:350–355 Google Scholar
- Miller F, Wang J, Zhu J, Chen Y, Hockenberry J (2017) Investigation of the Impact of the Massachusetts Health Care Reform on Hospital Costs and Quality of Care. Ann Oper Res 250:129–146. https://doi.org/10.1007/s10479-015-1856-yArticleGoogle Scholar
- de Almeida BL, Andrade MV, Guedes GR (2020) Brazilian hospitals’ performance: an assessment of the unified health system (SUS). Health Care Manag Sci 23:443–452. https://doi.org/10.1007/s10729-020-09505-5ArticleGoogle Scholar
- Gok MS, Altındağ E (2015) Analysis of the cost and efficiency relationship: experience in the Turkish pay for performance system. Eur J Health Econ 16:459–469. https://doi.org/10.1007/s10198-014-0584-6ArticleGoogle Scholar
- Li Y, Zhao Y, Xixin Niu, Zhou W, Tian J (2022) The efficiency evaluation of municipal-level traditional chinese medicine hospitals using data envelopment analysis after the implementation of hierarchical medical treatment policy in gansu province, china. INQUIRY 59:004695802210957. https://doi.org/10.1177/00469580221095799.
- Chang H, Chang W-J, Das S, Li S-H (2004) Health care regulation and the operating efficiency of hospitals: Evidence from Taiwan. J Account Public Policy 23:483–510. https://doi.org/10.1016/j.jaccpubpol.2004.10.004ArticleGoogle Scholar
- Cheng Z, Cai M, Tao H, He Z, Lin X, Lin H et al (2016) Efficiency and productivity measurement of rural township hospitals in China: a bootstrapping data envelopment analysis. BMJ Open 6:e011911. https://doi.org/10.1136/bmjopen-2016-011911ArticleGoogle Scholar
- Besstremyannaya G (2013) The impact of Japanese hospital financing reform on hospital efficiency: A difference-in-difference approach. Jpn Econ Rev 64:337–362. https://doi.org/10.1111/j.1468-5876.2012.00585.xArticleGoogle Scholar
- Tobin J (1958) Estimation of Relationships for Limited Dependent Variables. Econometrica 26:24–36. https://doi.org/10.2307/1907382ArticleGoogle Scholar
- López-Valcárcel B, Barber P (1996) Changes in the efficiency of Spanish public hospitals after the introduction of program-contracts. Investigaciones Economicas 20:377–402 Google Scholar
- Ozcan YA, Yeh S-C, McCollum D, Begun JW (1996) Trends in labor efficiency among American hospital markets. Ann Oper Res 67:61–81. https://doi.org/10.1007/BF02187024ArticleGoogle Scholar
- Burgess JF, Wilson PW (1998) Variation in inefficiency among us hospitals. INFOR: Information Systems and Operational Research 36:84–102. https://doi.org/10.1080/03155986.1998.11732348.
- Rego G, Nunes R, Costa J (2010) The challenge of corporatisation: the experience of Portuguese public hospitals. Eur J Health Econ 11:367–381. https://doi.org/10.1007/s10198-009-0198-6ArticleGoogle Scholar
- Sommersguter-Reichmann M (2000) The impact of the Austrian hospital financing reform on hospital productivity: empirical evidence on efficiency and technology changes using a non-parametric input-based Malmquist approach. Health Care Manag Sci. https://doi.org/10.1023/A:1019022230731
- Maniadakis N, Thanassoulis E (2000) Assessing productivity changes in UK hospitals reflecting technology and input prices. Appl Econ 32:1575–1589. https://doi.org/10.1080/000368400418970ArticleGoogle Scholar
- Chern JY, Wan TT (2000) The impact of the prospective payment system on the technical efficiency of hospitals. J Med Syst 24:159–172. https://doi.org/10.1023/a:1005542324990ArticleGoogle Scholar
- Peixoto MGM, Musetti MA, de Mendonça MCA (2020) Performance management in hospital organizations from the perspective of Principal Component Analysis and Data Envelopment Analysis: the case of Federal University Hospitals in Brazil. Comput Ind Eng 150:106873. https://doi.org/10.1016/j.cie.2020.106873ArticleGoogle Scholar
- Lobo MS de C, Rodrigues H de C, André ECG, de Azeredo JA, Lins MPE (2016) Dynamic network data envelopment analysis for university hospitals evaluation. Rev Saude Publica 50:22. https://doi.org/10.1590/S1518-8787.2016050006022.
- Chowdhury H, Zelenyuk V, Laporte A, Wodchis WP (2014) Analysis of productivity, efficiency and technological changes in hospital services in Ontario: How does case-mix matter? Int J Prod Econ 150:74–82. https://doi.org/10.1016/j.ijpe.2013.12.003ArticleGoogle Scholar
- Asmild M, Hollingsworth B, Birch S (2013) The scale of hospital production in different settings: one size does not fit all. J Prod Anal 40:197–206. https://doi.org/10.1007/s11123-012-0332-9ArticleGoogle Scholar
- Cheng Z, Tao H, Cai M, Lin H, Lin X, Shu Q et al (2015) Technical efficiency and productivity of Chinese county hospitals: an exploratory study in Henan province China. BMJ Open 5:e007267. https://doi.org/10.1136/bmjopen-2014-007267ArticleGoogle Scholar
- Li N-N, Wang C-H, Ni H, Wang H (2017) Efficiency and Productivity of County-level Public Hospitals Based on the Data Envelopment Analysis Model and Malmquist Index in Anhui China. Chin Med J (Engl) 130:2836–2843. https://doi.org/10.4103/0366-6999.219148ArticleGoogle Scholar
- Ng YC (2011) The productive efficiency of Chinese hospitals. China Econ Rev 22:428–439. https://doi.org/10.1016/j.chieco.2011.06.001ArticleGoogle Scholar
- Gai RY, Zhou CC, Xu LZ, Zhu M, Wang XZ, Li SX et al (2010) Health resource allocation and productive efficiency of Chinese county hospitals: data from 1993 to 2005. Biosci Trends 4:218–224 Google Scholar
- Yeşilyurt ME, Şahin E, Elbi MD, Kızılkaya A, Koyuncuoğlu MU, Akbaş-Yeşilyurt F (2021) A novel method for computing single output for DEA with application in hospital efficiency. Socioecon Plann Sci 76:100995. https://doi.org/10.1016/j.seps.2020.100995ArticleGoogle Scholar
- Jin F, Cai Y, Pedrycz W, Liu J (2022) Efficiency evaluation with regret-rejoice cross-efficiency DEA models under the distributed linguistic environment. Comput Ind Eng 169:108281. https://doi.org/10.1016/j.cie.2022.108281ArticleGoogle Scholar
- Castelli A, Street A, Verzulli R, Ward P (2015) Examining variations in hospital productivity in the English NHS. Eur J Health Econ 16:243–254. https://doi.org/10.1007/s10198-014-0569-5ArticleGoogle Scholar
- Asandului L, Roman M, Fatulescu P (2014) The Efficiency of Healthcare Systems in Europe: A Data Envelopment Analysis Approach. Procedia Economics and Finance 10:261–268. https://doi.org/10.1016/S2212-5671(14)00301-3ArticleGoogle Scholar
- Linna M, Häkkinen U (1999) Determinants of cost efficiency of Finnish hospitals: A comparison of DEA and SFA. Undefined
- Magnussen J (1996) Efficiency measurement and the operationalization of hospital production. Health Serv Res 31:21–37 Google Scholar
- Steinmann L, Dittrich G, Karmann A, Zweifel P (2004) Measuring and comparing the (in)efficiency of German and Swiss hospitals. Eur J Health Econom 5:216–226. https://doi.org/10.1007/s10198-004-0227-4ArticleGoogle Scholar
- Vera A, Kuntz L (2007) Process-based organization design and hospital efficiency. Health Care Manage Rev 32:55–65. https://doi.org/10.1097/00004010-200701000-00008ArticleGoogle Scholar
- Zarrin M, Schoenfelder J, Brunner JO (2022) Homogeneity and Best Practice Analyses in Hospital Performance Management: An Analytical Framework. Health Care Manag Sci 25:406–425. https://doi.org/10.1007/s10729-022-09590-8ArticleGoogle Scholar
- Aletras V, Kontodimopoulos N, Zagouldoudis A, Niakas D (2007) The short-term effect on technical and scale efficiency of establishing regional health systems and general management in Greek NHS hospitals. Health Policy 83:236–245. https://doi.org/10.1016/j.healthpol.2007.01.008ArticleGoogle Scholar
- Athanassopoulos AD, Gounaris C, Sissouras A (1999) A descriptive assessment of the production and cost efficiency of general hospitals in Greece. Health Care Manag Sci 2:97–106. https://doi.org/10.1023/a:1019023408924ArticleGoogle Scholar
- Flokou A, Kontodimopoulos N, Niakas D (2011) Employing post-DEA cross-evaluation and cluster analysis in a sample of Greek NHS hospitals. J Med Syst 35:1001–1014. https://doi.org/10.1007/s10916-010-9533-9ArticleGoogle Scholar
- Giokas DI (2001) Greek hospitals: how well their resources are used. Omega 29:73–83. https://doi.org/10.1016/S0305-0483(00)00031-1ArticleGoogle Scholar
- Kourtis M, Curtis P, Hanias M, Kourtis E (2021) A strategic financial management evaluation of private hospitals’ effectiveness and efficiency for sustainable financing: A Research Study. Eur Res Stud J XXIV:1025–54
- Kucsma D, Varga K (2021) Exploring effectiveness reserves in hospitals with the dea method. PFQ 66:75–87. https://doi.org/10.35551/PFQ_2021_s_2_4
- Jat TR, San Sebastian M (2013) Technical efficiency of public district hospitals in Madhya Pradesh, India: a data envelopment analysis. Glob Health Action 6:https://doi.org/10.3402/gha.v6i0.21742. https://doi.org/10.3402/gha.v6i0.21742.
- Mogha SK, Yadav SP, Singh SP (2015) Technical efficiency and productivity growth in public sector hospitals of Uttarakhand (India). Int J Syst Assur Eng Manag 6:390–406. https://doi.org/10.1007/s13198-014-0270-1ArticleGoogle Scholar
- Mogha SK, Yadav SP, Singh SP (2015) Slack based measure of efficiencies of public sector hospitals in Uttarakhand (India). Benchmarking: An International J 22:1229–46. https://doi.org/10.1108/BIJ-12-2013-0122.
- Prakash V, Annapoorni D (2015) Performance Evaluation of Public Hospitals in Tamil Nadu: DEA Approach. J Health Manag 17:417–424. https://doi.org/10.1177/0972063415606267ArticleGoogle Scholar
- Hatam N, Pourmohammadi K, Keshtkaran A, Javanbakht M, Askarian M (2012) Factors affecting efficiency of social security hospitals in Iran: Data Envelopment Analysis. HEALTHMED 6
- Jahangoshai Rezaee M, Karimdadi A, Izadbakhsh H (2019) Road map for progress and attractiveness of Iranian hospitals by integrating self-organizing map and context-dependent DEA. Health Care Manag Sci 22:410–436. https://doi.org/10.1007/s10729-019-09484-2ArticleGoogle Scholar
- Marnani A, Sadeghifar J, Pourmohammadi K, Mostafaie D, Abolhalaj M, Bastani P (2012) Performance assessment indicators: How DEA and Pabon Lasso describe Iranian hospitals’ performance. HealthMED 6:791–796 Google Scholar
- Mohamadi E, Kiani MM, Olyaeemanesh A, Takian A, Majdzadeh R, Hosseinzadeh Lotfi F et al (2022) Two-Step Estimation of the Impact of Contextual Variables on Technical Efficiency of Hospitals: The Case Study of Public Hospitals in Iran. Front Public Health 9:785489. https://doi.org/10.3389/fpubh.2021.785489ArticleGoogle Scholar
- Yusefzadeh H, Ghaderi H, Bagherzade R, Barouni M (2013) The efficiency and budgeting of public hospitals: case study of iran. Iran Red Crescent Med J 15:393–399. https://doi.org/10.5812/ircmj.4742ArticleGoogle Scholar
- Kordrostami S, Amirteimoori A, Jahani Sayyad Noveiri M (2019) Inputs and outputs classification in integer-valued data envelopment analysis. Measurement 139:317–25. https://doi.org/10.1016/j.measurement.2019.02.087
- Izadikhah M (2022) A fuzzy stochastic slacks-based data envelopment analysis model with application to healthcare efficiency. Healthcare Anal 2:100038. https://doi.org/10.1016/j.health.2022.100038ArticleGoogle Scholar
- Azadi M, Farzipoor SR (2013) A combination of QFD and imprecise DEA with enhanced Russell graph measure: A case study in healthcare. Socioecon Plann Sci 47:281–291. https://doi.org/10.1016/j.seps.2013.05.001ArticleGoogle Scholar
- Ghiyasi M, Soltanifar M, Sharafi H (2022) A novel inverse DEA-R model with application in hospital efficiency. Socio-Economic Planning Sciences 101427. https://doi.org/10.1016/j.seps.2022.101427.
- Omrani H, Shafaat K, Emrouznejad A (2018) An integrated fuzzy clustering cooperative game data envelopment analysis model with application in hospital efficiency. Expert Syst Appl 114:615–628. https://doi.org/10.1016/j.eswa.2018.07.074ArticleGoogle Scholar
- Omrani H, Alizadeh A, Emrouznejad A, Teplova T (2022) A robust credibility DEA model with fuzzy perturbation degree: An application to hospitals performance. Expert Syst Appl 189:116021. https://doi.org/10.1016/j.eswa.2021.116021ArticleGoogle Scholar
- Yang W, Cai L, Edalatpanah SA, Smarandache F (2020) Triangular Single Valued Neutrosophic Data Envelopment Analysis: Application to Hospital Performance Measurement. Symmetry 12:588. https://doi.org/10.3390/sym12040588ArticleGoogle Scholar
- Barbetta GP, Turati G, Zago AM (2007) Behavioral differences between public and private not-for-profit hospitals in the Italian national health service. Health Econ 16:75–96. https://doi.org/10.1002/hec.1143ArticleGoogle Scholar
- Mancuso P, Valdmanis VG (2016) Care Appropriateness and Health Productivity Evolution: A Non-Parametric Analysis of the Italian Regional Health Systems. Appl Health Econ Health Policy 14:595–607. https://doi.org/10.1007/s40258-016-0257-yArticleGoogle Scholar
- Matranga D, Sapienza F (2015) Congestion analysis to evaluate the efficiency and appropriateness of hospitals in Sicily. Health Policy 119:324–332. https://doi.org/10.1016/j.healthpol.2014.12.012ArticleGoogle Scholar
- Kawaguchi H, Tone K, Tsutsui M (2014) Estimation of the efficiency of Japanese hospitals using a dynamic and network data envelopment analysis model. Health Care Manag Sci 17:101–112. https://doi.org/10.1007/s10729-013-9248-9ArticleGoogle Scholar
- Zhang X, Tone K, Lu Y (2018) Impact of the Local Public Hospital Reform on the Efficiency of Medium-Sized Hospitals in Japan: An Improved Slacks-Based Measure Data Envelopment Analysis Approach. Health Serv Res 53:896–918. https://doi.org/10.1111/1475-6773.12676ArticleGoogle Scholar
- Najadat H, Alaiad A, Alasal SA, Mrayyan GA, Alsmadi I (2020) Integration of Data Envelopment Analysis and Clustering Methods. J Info Know Mgmt 19:2040006. https://doi.org/10.1142/S0219649220400067ArticleGoogle Scholar
- Munkhsaikhan S, Tsai A, Chang M-C (2011) Technical Efficiency of Public Hospitals in Mongolia. HealthMED 5:360–365 Google Scholar
- Silwal PR, Ashton T (2017) Productivity of public hospitals in Nepal: a data envelopment analysis. BMJ Open 7:e015327. https://doi.org/10.1136/bmjopen-2016-015327ArticleGoogle Scholar
- Ferrera J, Garcia A, Lau‐Cortés E, Polo C (2021) Assessing panamanian hospitals’ performance with alternative frontier methods. International Transactions in Operational Research 30. https://doi.org/10.1111/itor.13013
- Pederneiras YM, Pereira MA, Figueira JR (2023) Are the Portuguese public hospitals sustainable? A triple bottom line hybrid data envelopment analysis approach. Int Trans Oper Res 30:453–475. https://doi.org/10.1111/itor.12966ArticleGoogle Scholar
- Huang YG (1990) An application of data envelopment analysis: measuring the relative performance of Florida general hospitals. J Med Syst 14:191–196. https://doi.org/10.1007/BF00999268ArticleGoogle Scholar
- Chen H, Cates T, Taylor M, Cates C (2020) Improving the US hospital reimbursement: how patient satisfaction in HCAHPS reflects lower readmission. Int J Health Care Qual Assur 33:333–344. https://doi.org/10.1108/IJHCQA-03-2019-0066ArticleGoogle Scholar
- Peykani P, Mohammadi E, Emrouznejad A, Pishvaee MS, Rostamy-Malkhalifeh M (2019) Fuzzy data envelopment analysis: An adjustable approach. Expert Syst Appl 136:439–452. https://doi.org/10.1016/j.eswa.2019.06.039ArticleGoogle Scholar
- Peykani P, Memar-Masjed E, Arabjazi N, Mirmozaffari M (2022) Dynamic Performance Assessment of Hospitals by Applying Credibility-Based Fuzzy Window Data Envelopment Analysis. Healthcare 10:876. https://doi.org/10.3390/healthcare10050876ArticleGoogle Scholar
- Leleu H, Moises J, Valdmanis VG (2014) How do payer mix and technical inefficiency affect hospital profit? A weighted DEA approach. Oper Res Health Care 3:231–237. https://doi.org/10.1016/j.orhc.2014.06.002ArticleGoogle Scholar
- Kim Y, Lee K-H, Choi SW (2021) Multifaced Evidence of Hospital Performance in Pennsylvania. Healthcare 9:670. https://doi.org/10.3390/healthcare9060670ArticleGoogle Scholar
- Parkin D, Hollingsworth B (1997) Measuring production efficiency of acute hospitals in Scotland, 1991–94: validity issues in data envelopment analysis. Appl Econ 29:1425–1433. https://doi.org/10.1080/000368497326255ArticleGoogle Scholar
- Babalola TK, Moodley I (2020) Technical efficiency and productivity of public district hospitals in KwaZulu-Natal province South Africa. J Public Health Res 9:1741. https://doi.org/10.4081/jphr.2020.1741ArticleGoogle Scholar
- Martín J, Ortega-Díaz MI (2014) Hospital performance and benchmarking in spain. Annals of Management Science 3
- Prior D, Solà M (2000) Technical efficiency and economies of diversification in health care. Health Care Manag Sci 3:299–307. https://doi.org/10.1023/a:1019070113893ArticleGoogle Scholar
- Steinmann L, Zweifel P (2003) On the (in)efficiency of Swiss hospitals. Appl Econ 35:361–370. https://doi.org/10.1080/00036840210167183ArticleGoogle Scholar
- Hsiao B, Chen L-H (2019) Performance Evaluation for Taiwanese Hospitals by Multi-Activity Network Data Envelopment Analysis. Int J Info Tech Dec Mak 18:1009–1043. https://doi.org/10.1142/S0219622018500165ArticleGoogle Scholar
- Liu F-HF, Teng Y-H, Lai C-H (2011) The disaster response performance of hospitals in Taiwan: evaluation and classification. Qual Quant 45:495–511. https://doi.org/10.1007/s11135-010-9319-7
- Wen-Hsiang W, Chin-Tsai L, Zhi-Jun C, Kua-Hsin P (2011) Attaining Medical Care Resource Equity in Taiwan Using Grey Data Envelopment Analysis. J Grey Syst 23:201–210 Google Scholar
- Yeh D-Y, Cheng C-H (2016) Performance Management of Taiwan’s National Hospitals. Int J Info Tech Dec Mak 15:187–213. https://doi.org/10.1142/S0219622014500199ArticleGoogle Scholar
- Lin C-S, Chiu C-M, Huang Y-C, Lang H-C, Chen M-S (2021) Evaluating the Operational Efficiency and Quality of Tertiary Hospitals in Taiwan: The Application of the EBITDA Indicator to the DEA Method and TOBIT Regression. Healthcare 10:58. https://doi.org/10.3390/healthcare10010058ArticleGoogle Scholar
- Kao L, Lu C, Chiu C (2011) Efficiency measurement using independent component analysis and data envelopment analysis. Eur J Oper Res 210:310–317. https://doi.org/10.1016/j.ejor.2010.09.016ArticleGoogle Scholar
- Chang H (1998) Determinants of Hospital Efficiency: the Case of Central Government-owned Hospitals in Taiwan. Omega 26:307–317. https://doi.org/10.1016/S0305-0483(98)00014-0ArticleGoogle Scholar
- Fumbwe F, Lihawa R, Andrew F, Kinyanjui G, Mkuna E (2021) Examination on level of scale efficiency in public hospitals in Tanzania. Cost Eff Resour Alloc 19:49. https://doi.org/10.1186/s12962-021-00305-4ArticleGoogle Scholar
- Ersoy K, Kavuncubasi S, Ozcan YA, Harris JM (1997) Technical efficiencies of Turkish hospitals: DEA approach. J Med Syst 21:67–74. https://doi.org/10.1023/a:1022801222540ArticleGoogle Scholar
- Yildirim S, Kacak H, Yildirim C (2018) Reorganization health care delivery and productivity change: An assessment of turkish public hospital performance with malmquist index. J Appl Bus Econ 20. https://doi.org/10.33423/jabe.v20i3.510
- Girginer N, Köse T, Uçkun N (2015) Efficiency Analysis of Surgical Services by Combined Use of Data Envelopment Analysis and Gray Relational Analysis. J Med Syst 39:56. https://doi.org/10.1007/s10916-015-0238-yArticleGoogle Scholar
- Pham TL (2011) Efficiency and productivity of hospitals in Vietnam. J Health Organ Manag 25:195–213. https://doi.org/10.1108/14777261111134428ArticleGoogle Scholar
- Medin E, Häkkinen U, Linna M, Anthun KS, Kittelsen SAC, Rehnberg C et al (2013) International hospital productivity comparison: experiences from the Nordic countries. Health Policy 112:80–87. https://doi.org/10.1016/j.healthpol.2013.02.004ArticleGoogle Scholar
- Mobley LR, Magnussen J (1998) An international comparison of hospital efficiency: does institutional environment matter? Appl Econ 30:1089–1100. https://doi.org/10.1080/000368498325255ArticleGoogle Scholar
- Hollingsworth B, Parkin D (1995) The efficiency of Scottish acute hospitals: an application of data envelopment analysis. IMA J Math Appl Med Biol 12:161–173. https://doi.org/10.1093/imammb/12.3-4.161ArticleGoogle Scholar
- Linna M, Häkkinen U, Magnussen J (2006) Comparing hospital cost efficiency between Norway and Finland. Health Policy 77:268–278. https://doi.org/10.1016/j.healthpol.2005.07.019ArticleGoogle Scholar
- Linna M, Häkkinen U, Peltola M, Magnussen J, Anthun KS, Kittelsen S et al (2010) Measuring cost efficiency in the Nordic Hospitals—a cross-sectional comparison of public hospitals in 2002. Health Care Manag Sci 13:346–357. https://doi.org/10.1007/s10729-010-9134-7ArticleGoogle Scholar
- Kittelsen SAC, Magnussen J, Anthun KS, Häkkinen U, Linna M, Medin E et al (2008) Hospital productivity and the norwegian ownership reform: a Nordic comparative study. Helsinki: Stakes
- Kittelsen SAC, Winsnes BA, Anthun KS, Goude F, Hope Ø, Häkkinen U et al (2015) Decomposing the productivity differences between hospitals in the Nordic countries. J Prod Anal 43:281–293. https://doi.org/10.1007/s11123-015-0437-zArticleGoogle Scholar
- Kittelsen SAC, Anthun KS, Goude F, Huitfeldt IMS, Häkkinen U, Kruse M et al (2015) Costs and Quality at the Hospital Level in the Nordic Countries. Health Econ 24(Suppl 2):140–163. https://doi.org/10.1002/hec.3260ArticleGoogle Scholar
- Medin E, Anthun KS, Häkkinen U, Kittelsen SAC, Linna M, Magnussen J et al (2011) Cost efficiency of university hospitals in the Nordic countries: a cross-country analysis. Eur J Health Econ 12:509–519. https://doi.org/10.1007/s10198-010-0263-1ArticleGoogle Scholar
- Pilyavskyy A, Aaronson W, Matsiv Y (2017) Comparative Analysis Of Healthcare Performance In West And South Regions Of Ukraine. CER 19:143–155. https://doi.org/10.1515/cer-2016-0042ArticleGoogle Scholar
- Grosskopf S, Valdmanis V (1993) Evaluating hospital performance with case-mix-adjusted outputs. Med Care 31:525–532. https://doi.org/10.1097/00005650-199306000-00006ArticleGoogle Scholar
- Barros PP, Brouwer WBF, Thomson S, Varkevisser M (2016) Competition among health care providers: helpful or harmful? Eur J Health Econ 17:229–233. https://doi.org/10.1007/s10198-015-0736-3ArticleGoogle Scholar
- Herr A, Schmitz H, Augurzky B (2011) Profit efficiency and ownership of German hospitals. Health Econ 20:660–674. https://doi.org/10.1002/hec.1622ArticleGoogle Scholar
- Chirikos TN, Sear AM (1994) Technical efficiency and the competitive behavior of hospitals. Socioecon Plann Sci 28:219–227 ArticleGoogle Scholar
- Lee K-H, Park J, Lim S, Park S-C (2015) Has Competition Increased Hospital Technical Efficiency? Health News 34:106–112. https://doi.org/10.1097/HCM.0000000000000061ArticleGoogle Scholar
- Dalmau E, Puig-Junoy J (1997) Market structure and hospital efficiency: Evaluating potential effects of deregulation in a national health service. Rochester, NY: Social Science Research Network
- Bates LJ, Mukherjee K, Santerre RE (2006) Market Structure and Technical Efficiency in the Hospital Services Industry: A DEA Approach. Med Care Res Rev 63:499–524. https://doi.org/10.1177/1077558706288842ArticleGoogle Scholar
- Tiemann O, Schreyögg J (2012) Changes in hospital efficiency after privatization. Health Care Manag Sci 15:310–326. https://doi.org/10.1007/s10729-012-9193-zArticleGoogle Scholar
- Alonso JM, Clifton J, Díaz-Fuentes D (2015) The impact of New Public Management on efficiency: an analysis of Madrid’s hospitals. Health Policy 119:333–340. https://doi.org/10.1016/j.healthpol.2014.12.001ArticleGoogle Scholar
- van Ineveld M, van Oostrum J, Vermeulen R, Steenhoek A, van de Klundert J (2016) Productivity and quality of Dutch hospitals during system reform. Health Care Manag Sci 19:279–290. https://doi.org/10.1007/s10729-015-9321-7ArticleGoogle Scholar
- Li SK, He X (2019) The impacts of marketization and subsidies on the treatment quality performance of the Chinese hospitals sector. China Econ Rev 54:41–50. https://doi.org/10.1016/j.chieco.2018.10.007ArticleGoogle Scholar
- Jha AK, Doolan D, Grandt D, Scott T, Bates DW (2008) The use of health information technology in seven nations. Int J Med Inform 77:848–854. https://doi.org/10.1016/j.ijmedinf.2008.06.007ArticleGoogle Scholar
- Pai DR, Rajan B, Chakraborty S (2022) Do EHR and HIE deliver on their promise? Analysis of Pennsylvania acute care hospitals. Int J Prod Econ 245:108398. https://doi.org/10.1016/j.ijpe.2021.108398ArticleGoogle Scholar
- Himmelstein DU, Jun M, Busse R, Chevreul K, Geissler A, Jeurissen P et al (2014) A comparison of hospital administrative costs in eight nations: US costs exceed all others by far. Health Aff (Millwood) 33:1586–1594. https://doi.org/10.1377/hlthaff.2013.1327ArticleGoogle Scholar
- Lin Y-K, Lin M, Chen H (2019) Do Electronic Health Records Affect Quality of Care? Evidence from the HITECH Act. Inf Syst Res 30:306–318. https://doi.org/10.1287/isre.2018.0813ArticleGoogle Scholar
- Watcharasriroj B, Tang J (2004) The effects of size and information technology on hospital efficiency. J High Technol Managem Res 15:1–16. https://doi.org/10.1016/j.hitech.2003.09.001ArticleGoogle Scholar
- Kazley AS, Ozcan YA (2009) Electronic medical record use and efficiency: A DEA and windows analysis of hospitals. Socioecon Plann Sci 43:209–216. https://doi.org/10.1016/j.seps.2008.10.001ArticleGoogle Scholar
- Huerta TR, Thompson MA, Ford EW, Ford WF (2013) Implementing electronic lab order entry management in hospitals: Incremental strategies lead to better productivity outcomes. Int J Inf Manage 33:40–47. https://doi.org/10.1016/j.ijinfomgt.2012.05.008ArticleGoogle Scholar
- Williams C, Asi Y, Raffenaud A, Bagwell M, Zeini I (2016) The effect of information technology on hospital performance. Health Care Manag Sci 19:338–346. https://doi.org/10.1007/s10729-015-9329-zArticleGoogle Scholar
- Cho N-E, Chang J, Atems B (2014) The effects of health information technology adoption and hospital-physician integration on hospital efficiency. Am J Manag Care 20:eSP9–15
- Pai DR, Hosseini H, Brown RS (2019) Does efficiency and quality of care affect hospital closures? Health Syst (Basingstoke) 8:17–30. https://doi.org/10.1080/20476965.2017.1405874ArticleGoogle Scholar
- Butler TW, Li L (2005) The utility of returns to scale in DEA programming: An analysis of Michigan rural hospitals. Eur J Oper Res 161:469–477. https://doi.org/10.1016/j.ejor.2003.09.019ArticleGoogle Scholar
- Banker RD, Charnes A, Cooper WW (1984) Some Models for Estimating Technical and Scale Inefficiencies in Data Envelopment Analysis. Manage Sci 30:1078–1092 ArticleGoogle Scholar
- Nayar P, Ozcan YA, Yu F, Nguyen AT (2013) Benchmarking urban acute care hospitals: efficiency and quality perspectives. Health Care Manage Rev 38:137–145. https://doi.org/10.1097/HMR.0b013e3182527a4cArticleGoogle Scholar
- Li B, Mohiuddin M, Liu Q (2019) Determinants and Differences of Township Hospital Efficiency among Chinese Provinces. Int J Environ Res Public Health 16:1601. https://doi.org/10.3390/ijerph16091601ArticleGoogle Scholar
- Rezaee MJ, Karimdadi A (2015) Do Geographical Locations Affect in Hospitals Performance? A Multi-group Data Envelopment Analysis. J Med Syst 39:85. https://doi.org/10.1007/s10916-015-0278-3ArticleGoogle Scholar
- Nedelea IC, Fannin JM (2013) Impact of conversion to Critical Access Hospital status on hospital efficiency. Socioecon Plann Sci 47:258–269. https://doi.org/10.1016/j.seps.2012.09.005ArticleGoogle Scholar
- Nedelea C, Fannin M (2013) Analyzing cost efficiency of Critical Access Hospitals. J Policy Model 35:183–195. https://doi.org/10.1016/j.jpolmod.2012.10.002ArticleGoogle Scholar
- Nedelea IC, Fannin JM (2017) Testing for cost efficiency differences between two groups of rural hospitals. Intl J Healthcare Manage 10:57–65. https://doi.org/10.1080/20479700.2016.1259146ArticleGoogle Scholar
- Gautam S, Hicks L, Johnson T, Mishra B (2013) Measuring the Performance of Critical Access Hospitals in Missouri Using Data Envelopment Analysis. J Rural Health 29:150–158. https://doi.org/10.1111/j.1748-0361.2012.00439.xArticleGoogle Scholar
- Chu H-L, Liu S-Z, Romeis JC (2002) Does the Implementation of Responsibility Centers, Total Quality Management, and Physician Fee Programs Improve Hospital Efficiency?: Evidence from Taiwan Hospitals. Med Care 40:1223–1237 ArticleGoogle Scholar
- Prior D (2006) Efficiency and total quality management in health care organizations: A dynamic frontier approach. Annals OR 145:281–299. https://doi.org/10.1007/s10479-006-0035-6ArticleGoogle Scholar
- Lindlbauer I, Schreyögg J, Winter V (2016) Changes in technical efficiency after quality management certification: A DEA approach using difference-in-difference estimation with genetic matching in the hospital industry. Eur J Oper Res 250:1026–1036. https://doi.org/10.1016/j.ejor.2015.10.029ArticleGoogle Scholar
- Chang S-J, Hsiao H-C, Huang L-H, Chang H (2011) Taiwan quality indicator project and hospital productivity growth. Omega 39:14–22. https://doi.org/10.1016/j.omega.2010.01.006ArticleGoogle Scholar
- Morey RC, Fine DJ, Loree SW, Retzlaff-Roberts DL, Tsubakitani S (1992) The trade-off between hospital cost and quality of care An exploratory empirical analysis. Med Care 30:677–698. https://doi.org/10.1097/00005650-199208000-00002ArticleGoogle Scholar
- Chang L, Lan Y-W (2010) Has the National Health Insurance Scheme improved hospital efficiency in Taiwan? Identifying factors that affects its efficiency. Afr J Bus Manage 4:3752–3760 Google Scholar
- Gonçalves AC, Almeida RMVR, Lins MPE, Samanez CP (2013) Canonical correlation analysis in the definition of weight restrictions for data envelopment analysis. J Appl Stat 40:1032–1043. https://doi.org/10.1080/02664763.2013.772571ArticleGoogle Scholar
- Gholami R, Añón Higón D, Emrouznejad A (2015) Hospital performance: Efficiency or quality? Can we have both with IT? Expert Syst Appl 42:5390–5400. https://doi.org/10.1016/j.eswa.2014.12.019ArticleGoogle Scholar
- Morey RC, Retzlaff-Roberts DL, Fine DJ (1994) Getting Something for Nothing: Estimating Service Level Improvements Possible in Hospitals. Int Trans Operational Res 1:285–292. https://doi.org/10.1111/1475-3995.d01-40ArticleGoogle Scholar
- Hu H-H, Qi Q, Yang C-H (2012) Evaluation of China’s regional hospital efficiency: DEA approach with undesirable output. J Oper Res Soc 63:715–725 ArticleGoogle Scholar
- Sahin I, Ozcan YA (2000) Public sector hospital efficiency for provincial markets in Turkey. J Med Syst 24:307–320. https://doi.org/10.1023/a:1005576009257ArticleGoogle Scholar
- Varabyova Y, Schreyögg J (2013) International comparisons of the technical efficiency of the hospital sector: panel data analysis of OECD countries using parametric and non-parametric approaches. Health Policy 112:70–79. https://doi.org/10.1016/j.healthpol.2013.03.003ArticleGoogle Scholar
- Guo H, Zhao Y, Niu T, Tsui K-L (2017) Hong Kong Hospital Authority resource efficiency evaluation: Via a novel DEA-Malmquist model and Tobit regression model. PLoS ONE 12:e0184211. https://doi.org/10.1371/journal.pone.0184211ArticleGoogle Scholar
- Campanella P, Azzolini E, Izzi A, Pelone F, De Meo C, La Milia D et al (2017) Hospital efficiency: how to spend less maintaining quality? Ann Ist Super Sanita 53:46–53. https://doi.org/10.4415/ANN_17_01_10ArticleGoogle Scholar
- Raei B, Yousofi M, Rahmani K, Afshari S, Ameri H (2017) Patterns of productivity changes in hospitals by using Malmquist - DEA Index: A panel data analysis (2011–2016). Australasian Medical J 10. https://doi.org/10.21767/AMJ.2017.3094.
- Gong G, Chen Y, Gao H, Su D, Chang J (2019) Has the Efficiency of China’s Healthcare System Improved after Healthcare Reform? A Network Data Envelopment Analysis and Tobit Regression Approach. Int J Environ Res Public Health 16:4847. https://doi.org/10.3390/ijerph16234847ArticleGoogle Scholar
- Alatawi AD, Niessen LW, Khan JAM (2020) Efficiency evaluation of public hospitals in Saudi Arabia: an application of data envelopment analysis. BMJ Open 10:e031924. https://doi.org/10.1136/bmjopen-2019-031924ArticleGoogle Scholar
- Barpanda S, Sreekumar N (2020) Performance Analysis of Hospitals in Kerala Using Data Envelopment Analysis Model. J Health Manag 22:25–40. https://doi.org/10.1177/0972063420908372ArticleGoogle Scholar
- Şahin B, İlgün G, Sönmez S (2021) Determining the factors affecting the technical efficiency scores of public hospitals using different regression methods. Benchmarking: Intl J 28:2202–15. https://doi.org/10.1108/BIJ-08-2020-0427.
- Yin G, Chen C, Zhuo L, He Q, Tao H (2021) Efficiency Comparison of Public Hospitals under Different Administrative Affiliations in China: A Pilot City Case. Healthcare (Basel) 9:437. https://doi.org/10.3390/healthcare9040437ArticleGoogle Scholar
- Orsini LP, Leardini C, Vernizzi S, Campedelli B (2021) Inefficiency of public hospitals: a multistage data envelopment analysis in an Italian region. BMC Health Serv Res 21:1281. https://doi.org/10.1186/s12913-021-07276-5ArticleGoogle Scholar
- Noveiri M, Kordrostami S (2021) Sustainability assessment using a fuzzy DEA aggregation approach: a healthcare application. Soft Comput 25:10829–10849. https://doi.org/10.1007/s00500-021-05992-yArticleGoogle Scholar
- Yang J, Zeng W (2014) The trade-offs between efficiency and quality in the hospital production: Some evidence from Shenzhen China. China Economic Review 31:166–184. https://doi.org/10.1016/j.chieco.2014.09.005ArticleGoogle Scholar
- Ortega-Díaz MI, Martín JC (2022) How to detect hospitals where quality would not be jeopardized by health cost savings? A methodological approach using DEA with SBM analysis. Health Policy 126:1069–1074. https://doi.org/10.1016/j.healthpol.2022.07.010ArticleGoogle Scholar
- Kheirollahi H, Hessari P, Charles V, Chawshini R (2017) An input relaxation model for evaluating congestion in fuzzy DEA. Croatian Operational Research Review 8:391–408. https://doi.org/10.17535/crorr.2017.0025
- Nayar P, Ozcan YA (2008) Data Envelopment Analysis Comparison of Hospital Efficiency and Quality. J Med Syst 32:193–199. https://doi.org/10.1007/s10916-007-9122-8ArticleGoogle Scholar
- Huerta TR, Ford EW, Peterson LT, Brigham KH (2008) Testing the hospital value proposition: An empirical analysis of efficiency and quality. Health Care Manage Rev 33:341–349. https://doi.org/10.1097/01.HCM.0000318770.82642.c6ArticleGoogle Scholar
- Clement JP, Valdmanis VG, Bazzoli GJ, Zhao M, Chukmaitov A (2008) Is more better? An analysis of hospital outcomes and efficiency with a DEA model of output congestion. Health Care Manage Sci 11:67–77. https://doi.org/10.1007/s10729-007-9025-8ArticleGoogle Scholar
- Choi JH, Park I, Jung I, Dey A (2017) Complementary effect of patient volume and quality of care on hospital cost efficiency. Health Care Manag Sci 20:221–231. https://doi.org/10.1007/s10729-015-9348-9ArticleGoogle Scholar
- Roth A, Tucker AL, Venkataraman S, Chilingerian J (2019) Being on the Productivity Frontier: Identifying “Triple Aim Performance” Hospitals. Prod Oper Manag 28:2165–2183. https://doi.org/10.1111/poms.13019ArticleGoogle Scholar
- Pitocco C, Sexton TR, Stickle K (2020) Using Data Analytics to Improve Hospital Quality Performance. J Healthc Manag 65:285. https://doi.org/10.1097/JHM-D-19-00118ArticleGoogle Scholar
- Onder O, Cook W, Kristal M (2022) Does quality help the financial viability of hospitals? A data envelopment analysis approach. Socioecon Plann Sci 79:101105. https://doi.org/10.1016/j.seps.2021.101105ArticleGoogle Scholar
- Leleu H, Al-Amin M, Rosko M, Valdmanis VG (2018) A robust analysis of hospital efficiency and factors affecting variability. Health Serv Manage Res 31:33–42. https://doi.org/10.1177/0951484817730537ArticleGoogle Scholar
- Khushalani J, Ozcan YA (2017) Are hospitals producing quality care efficiently? An analysis using Dynamic Network Data Envelopment Analysis (DEA). Socioecon Plann Sci 60:15–23. https://doi.org/10.1016/j.seps.2017.01.009ArticleGoogle Scholar
- Valdmanis VG, Rosko MD, Mutter RL (2008) Hospital Quality, Efficiency, and Input Slack Differentials. Health Serv Res 43:1830–1848. https://doi.org/10.1111/j.1475-6773.2008.00893.xArticleGoogle Scholar
- Gok MS, Sezen B (2013) Analyzing the ambiguous relationship between efficiency, quality and patient satisfaction in healthcare services: The case of public hospitals in Turkey. Health Policy 111:290–300. https://doi.org/10.1016/j.healthpol.2013.05.010ArticleGoogle Scholar
- Ferrier GD, Trivitt JS (2013) Incorporating quality into the measurement of hospital efficiency: a double DEA approach. J Prod Anal 40:337–355. https://doi.org/10.1007/s11123-012-0305-zArticleGoogle Scholar
- Laine J, Linna M, Häkkinen U, Noro A (2005) Measuring the productive efficiency and clinical quality of institutional long-term care for the elderly: Long-Term Care of the Elderly. Health Econ 14:245–256. https://doi.org/10.1002/hec.926ArticleGoogle Scholar
- Jahantigh F, Ostovare M (2020) Application of a Hybrid Method for Performance Evaluation of Teaching Hospitals in Tehran. Qual Manag Health Care 29:210–217. https://doi.org/10.1097/QMH.0000000000000265ArticleGoogle Scholar
- Mitropoulos P (2022) A metafrontier Global Malmquist framework for hospitals productivity and quality measurement: Evidence from the Greek economic recession. EURO J Decision Process 10:100018. https://doi.org/10.1016/j.ejdp.2022.100018ArticleGoogle Scholar
- Mirmozaffari M, Yazdani R, Shadkam E, Khalili SM, Tavassoli LS, Boskabadi A (2021) A Novel Hybrid Parametric and Non-Parametric Optimisation Model for Average Technical Efficiency Assessment in Public Hospitals during and Post-COVID-19 Pandemic. Bioengineering 9:7. https://doi.org/10.3390/bioengineering9010007ArticleGoogle Scholar
- Caunic R-E, Asandului L, Bedrule-Grigoruță MV (2021) A Data Envelopment Analysis Of The Response Of Healthcare Facilities To Coronavirus Pandemic: Evidence From Romania. EURINT 8:23–40 Google Scholar
- Nepomuceno TCC, Silva WMN, Nepomuceno KTC, Barros IKF (2020) A DEA-Based Complexity of Needs Approach for Hospital Beds Evacuation during the COVID-19 Outbreak. J Healthcare Eng 2020:e8857553. https://doi.org/10.1155/2020/8857553ArticleGoogle Scholar
- Soroush F, Nabilou B, Faramarzi A, Yusefzadeh H (2022) A study of the evacuation and allocation of hospital beds during the Covid-19 epidemic: a case study in Iran. BMC Health Serv Res 22:864. https://doi.org/10.1186/s12913-022-08286-7ArticleGoogle Scholar
- Sun M, Ye Y, Zhang G, Xue Y, Shang X (2023) Measuring the efficiency of public hospitals: A multistage data envelopment analysis in Fujian Province, China. Frontiers in Public Health 11
- Henriques CO, Gouveia MC (2022) Assessing the impact of COVID-19 on the efficiency of Portuguese state-owned enterprise hospitals. Socio-Economic Planning Sciences 101387. https://doi.org/10.1016/j.seps.2022.101387.
- Kamel MA, Mousa ME-S (2021) Measuring operational efficiency of isolation hospitals during COVID-19 pandemic using data envelopment analysis: a case of Egypt. Benchmarking: Intl J 28:2178–201. https://doi.org/10.1108/BIJ-09-2020-0481
- Shahian DM, Nordberg P, Meyer GS, Blanchfield BB, Mort EA, Torchiana DF et al (2012) Contemporary performance of U.S. teaching and nonteaching hospitals. Acad Med 87:701–8. https://doi.org/10.1097/ACM.0b013e318253676a
- Sherman HD (1984) Hospital efficiency measurement and evaluation. Empirical test of a new technique. Med Care 22:922–38. https://doi.org/10.1097/00005650-198410000-00005
- Morey RC, Ozcan YA, Retzlaff-Roberts DL, Fine DJ (1995) Estimating the hospital-wide cost differentials warranted for teaching hospitals. An alternative to regression approaches. Med Care 33:531–52. https://doi.org/10.1097/00005650-199505000-00007
- Grosskopf S, Margaritis D, Valdmanis V (2004) Competitive effects on teaching hospitals. Eur J Oper Res 154:515–525. https://doi.org/10.1016/S0377-2217(03)00185-1ArticleGoogle Scholar
- Gok SM, Sezen B (2012) Capacity inefficiencies of teaching and non-teaching hospitals. Serv Ind J 32:2307–2328. https://doi.org/10.1080/02642069.2011.582495ArticleGoogle Scholar
- Yildirim C, Kacak H, Yildirim S, Kavuncubasi S (2019) Comprehensive efficiency assessment of turkish teaching hospitals: Technical, pure technical and scale efficiencies with data envelopment analysis. J Appl Business Econ 21. https://doi.org/10.33423/jabe.v21i3.2087
- Grosskopf S, Margaritis D, Valdmanis V (2001) Comparing teaching and non-teaching hospitals: a frontier approach (teaching vs. non-teaching hospitals). Health Care Manag Sci 4:83–90. https://doi.org/10.1023/a:1011449425940
- Harrison JP, Lambiase LR (2007) The Improving Efficiency of University Health Consortium Hospitals. J Public Budg Account Financ Manag 19:385–399. https://doi.org/10.1108/JPBAFM-19-03-2007-B007ArticleGoogle Scholar
- Torabipour A, Najarzadeh M, Arab M, Farzianpour F, Ghasemzadeh R (2014) Hospitals Productivity Measurement Using Data Envelopment Analysis Technique. Iran J Public Health 43:1576–1581 Google Scholar
- Pai DR, Dissanayake CK, Anna AM (2023) A comparison of critical access hospitals and other rural acute care hospitals in Pennsylvania. J Rural Health https://doi.org/10.1111/jrh.12755
- Harris J, Ozgen H, Ozcan Y (2000) Do Mergers Enhance the Performance of Hospital Efficiency? J Oper Res Soc 51:801–811. https://doi.org/10.2307/253961ArticleGoogle Scholar
- Ferrier GD, Valdmanis VG (2004) Do Mergers Improve Hospital Productivity? J Oper Res Soc 55:1071–1080 ArticleGoogle Scholar
- Groff JE, Lien D, Su J (2007) Measuring Efficiency Gains from Hospital Mergers. Res Healthcare Financial Manage 11:77–90 Google Scholar
- Kristensen T, Bogetoft P, Pedersen KM (2010) Potential gains from hospital mergers in Denmark. Health Care Manag Sci 13:334–345. https://doi.org/10.1007/s10729-010-9133-8ArticleGoogle Scholar
- Kjekshus L, Hagen T (2007) Do hospital mergers increase hospital efficiency? Evidence from a National Health Service country. J Health Serv Res Policy 12:230–235. https://doi.org/10.1258/135581907782101561ArticleGoogle Scholar
- Flokou A, Aletras V, Niakas D (2017) Decomposition of potential efficiency gains from hospital mergers in Greece. Health Care Manag Sci 20:467–484. https://doi.org/10.1007/s10729-016-9365-3ArticleGoogle Scholar
- Büchner VA, Hinz V, Schreyögg J (2016) Health systems: changes in hospital efficiency and profitability. Health Care Manag Sci 19:130–143. https://doi.org/10.1007/s10729-014-9303-1ArticleGoogle Scholar
- Giménez V, Prior D, Keith JR (2020) Strategic alliances’ effects over hospital efficiency and capacity utilization in México. Academia Revista Latinoamericana de Administración 33:128–146. https://doi.org/10.1108/ARLA-11-2018-0248ArticleGoogle Scholar
- Athanassopoulos A, Gounaris C (2001) Assessing the technical and allocative efficiency of hospital operations in Greece and its resource allocation implications. Eur J Oper Res 133:416–431. https://doi.org/10.1016/S0377-2217(00)00180-6ArticleGoogle Scholar
- Hofmarcher MM, Paterson I, Riedel M (2002) Measuring hospital efficiency in Austria–a DEA approach. Health Care Manag Sci 5:7–14. https://doi.org/10.1023/a:1013292801100ArticleGoogle Scholar
- Ramanathan R (2005) Operations assessment of hospitals in the Sultanate of Oman. Int J Oper Prod Manag 25:39–54. https://doi.org/10.1108/01443570510572231ArticleGoogle Scholar
- Morey RC, Fine D, Loree S (1990) Comparing the allocative efficiencies of hospitals. Omega 18:71–83. https://doi.org/10.1016/0305-0483(90)90019-6ArticleGoogle Scholar
- Puig-Junoy J (2000) Partitioning input cost efficiency into its allocative and technical components: An empirical DEA application to hospitals. Socioecon Plann Sci 34:199–218. https://doi.org/10.1016/S0038-0121(99)00024-5ArticleGoogle Scholar
- Olesen O, Petersen N (2002) The Use of Data Envelopment Analysis with Probabilistic Assurance Regions for Measuring Hospital Efficiency. J Prod Anal 17:83–109 ArticleGoogle Scholar
- Andersen P, Petersen NC (1993) A Procedure for Ranking Efficient Units in Data Envelopment Analysis. Manage Sci 39:1261–1264 ArticleGoogle Scholar
- Dittman DA, Capettini R, Morey RC (1991) Measuring efficiency in acute care hospitals: an application of data envelopment analysis. J Health Hum Resour Adm 14:89–108 Google Scholar
- Valdmanis V (1992) Sensitivity analysis for DEA models: An empirical example using public vs. NFP hospitals. J Public Econ 48:185–205. https://doi.org/10.1016/0047-2727(92)90026-CArticleGoogle Scholar
- Cudney EA, Baru RA, Guardiola I, Materla T, Cahill W, Phillips R et al (2019) A decision support simulation model for bed management in healthcare. Int J Health Care Qual Assur 32:499–515. https://doi.org/10.1108/IJHCQA-10-2017-0186ArticleGoogle Scholar
- Green L (2006) Queueing analysis in healthcare. In: Hall RW (ed). Patient Flow: Reducing Delay in Healthcare Delivery, Boston, MA: Springer US; p. 281–307. https://doi.org/10.1007/978-0-387-33636-7_10
- Cochran JK, Roche K (2008) A queuing-based decision support methodology to estimate hospital inpatient bed demand. J Oper Res Soc 59:1471–1482. https://doi.org/10.1057/palgrave.jors.2602499ArticleGoogle Scholar
- Lee S-Y, Chinnam RB, Dalkiran E, Krupp S, Nauss M (2021) Proactive coordination of inpatient bed management to reduce emergency department patient boarding. Int J Prod Econ 231:107842. https://doi.org/10.1016/j.ijpe.2020.107842ArticleGoogle Scholar
- Nguyen K-H, Coelli T (2009) Quantifying the effects of modelling choices on hospital efficiency measures: A meta-regression analysis 62
- Matos R, Ferreira Diogo, Pedro Maria Isabel (2021) Economic analysis of portuguese public hospitals through the construction of quality, efficiency, access, and financial related composite indicators. Soc Indic Res 157:361–92. https://doi.org/10.1007/s11205-021-02650-6.
- Kakemam E, Goodall AH (2019) Hospital performance and clinical leadership: new evidence from Iran. BMJ Leader 3. https://doi.org/10.1136/leader-2019-000160
- Kiani MM, Raei B, Asbagharani PA, Yousefi M, Rigi SAM, Salehi M et al (2018) Comparison of the technical efficiency of the hospital sector: Panel data analysis of the Iranian hospitals using parametric and non-parametric approaches. Bali Med J 8:114. https://doi.org/10.15562/bmj.v8i1.1242
- Choi JH, Fortsch SM, Park I, Jung I (2017) Efficiency of U.S. hospitals between 2001 and 2011. Manag Decis Econ 38:1071–81. https://doi.org/10.1002/mde.2846
- Blatnik P, Bojnec Š, Tušak M (2017) Measuring Efficiency of Secondary Healthcare Providers in Slovenia. Open Med (Wars) 12:214–225. https://doi.org/10.1515/med-2017-0031ArticleGoogle Scholar
- Chen Z, Chen X, Gan X, Bai K, Baležentis T, Cui L (2020) Technical Efficiency of Regional Public Hospitals in China Based on the Three-Stage DEA. Int J Environ Res Public Health 17:9383. https://doi.org/10.3390/ijerph17249383ArticleGoogle Scholar
- Chirikos TN, Sear AM (2000) Measuring hospital efficiency: a comparison of two approaches. Health Serv Res 34:1389–1408 Google Scholar
- Linna M (1998) Measuring hospital cost efficiency with panel data models. Health Econ 7:415–427. https://doi.org/10.1002/(sici)1099-1050(199808)7:5%3c415::aid-hec357%3e3.0.co;2-9ArticleGoogle Scholar
- Coelli T, Prasada Rao DS, O’Donnell CJ, Battese GE (2005) An introduction to efficiency and productivity analysis, 2nd edn. Springer, New York Google Scholar
- Jacobs R (2001) Alternative Methods to Examine Hospital Efficiency: Data Envelopment Analysis and Stochastic Frontier Analysis. Health Care Manag Sci 4:103–115. https://doi.org/10.1023/A:1011453526849ArticleGoogle Scholar
- Simões P, Marques RC (2011) Performance and congestion analysis of the portuguese hospital services. Cent Eur J Oper Res 19:39–63. https://doi.org/10.1007/s10100-009-0122-2ArticleGoogle Scholar
- Ferrier GD, Rosko MD, Valdmanis VG (2006) Analysis of uncompensated hospital care using a DEA model of output congestion. Health Care Manag Sci 9:181–188. https://doi.org/10.1007/s10729-006-7665-8ArticleGoogle Scholar
- Masiye F (2007) Investigating health system performance: An application of data envelopment analysis to Zambian hospitals. BMC Health Serv Res 7:58. https://doi.org/10.1186/1472-6963-7-58ArticleGoogle Scholar
- Dehnokhalaji A, Khezri S, Emrouznejad A (2022) A box-uncertainty in DEA: A robust performance measurement framework. Expert Syst Appl 187:115855. https://doi.org/10.1016/j.eswa.2021.115855ArticleGoogle Scholar
- Wu D, Wu DD (2019) Risk-Based Robust Evaluation of Hospital Efficiency. IEEE Syst J 13:1906–1914. https://doi.org/10.1109/JSYST.2018.2865031ArticleGoogle Scholar
- Hajialiafzali H, Moss JR, Mahmood MA (2007) Efficiency measurement for hospitals owned by the Iranian social security organisation. J Med Syst 31:166–172. https://doi.org/10.1007/s10916-007-9051-6ArticleGoogle Scholar
- Hatam N (2008) The Role of Data Envelopment Analysis (DEA) Pattern in the Efficiency of Social Security Hospitals in Iran. Iran Red Crescent Med J 10:208–214 Google Scholar
- Hatam N, Moslehi S, Askarian M, Shokrpour N, Keshtkaran A, Abbasi M (2010) The Efficiency of General Public Hospitals in Fars Province, Southern Iran. Iran Red Crescent Med J 12:138–144 Google Scholar
- Kirigia J, Emrouznejad A, Cassoma B, Zere E, Barry S (2009) A Performance Assessment Method for Hospitals: The Case of Municipal Hospitals in Angola. J Med Syst 32:509–519. https://doi.org/10.1007/s10916-008-9157-5ArticleGoogle Scholar
- Kontodimopoulos N, Nanos P, Niakas D (2006) Balancing efficiency of health services and equity of access in remote areas in Greece. Health Policy 76:49–57. https://doi.org/10.1016/j.healthpol.2005.04.006ArticleGoogle Scholar
- Ozcan YA, Lins ME, Lobo MSC, da Silva ACM, Fiszman R, Pereira BB (2010) Evaluating the performance of Brazilian university hospitals. Ann Oper Res 178:247–261. https://doi.org/10.1007/s10479-009-0528-1ArticleGoogle Scholar
- Pilyavsky AI, Aaronson WE, Bernet PM, Rosko MD, Valdmanis VG, Golubchikov MV (2006) East–west: does it make a difference to hospital efficiencies in Ukraine? Health Econ 15:1173–1186. https://doi.org/10.1002/hec.1120ArticleGoogle Scholar
- Pilyavsky A, Staat M (2006) Health care in the CIS countries : the case of hospitals in Ukraine. Eur J Health Econ 7:189–195. https://doi.org/10.1007/s10198-006-0351-4ArticleGoogle Scholar
- Vitikainen K, Street A, Linna M (2009) Estimation of hospital efficiency—Do different definitions and casemix measures for hospital output affect the results? Health Policy 89:149–159. https://doi.org/10.1016/j.healthpol.2008.05.012ArticleGoogle Scholar
- Blank JLT, Valdmanis VG (2010) Environmental factors and productivity on Dutch hospitals: a semi-parametric approach. Health Care Manag Sci 13:27–34. https://doi.org/10.1007/s10729-009-9104-0ArticleGoogle Scholar
- Puenpatom RA, Rosenman R (2008) Efficiency of Thai provincial public hospitals during the introduction of universal health coverage using capitation. Health Care Manage Sci 11:319–338. https://doi.org/10.1007/s10729-008-9057-8ArticleGoogle Scholar
- Staat M (2006) Efficiency of hospitals in Germany: a DEA-bootstrap approach. Appl Econ 38:2255–2263. https://doi.org/10.1080/00036840500427502ArticleGoogle Scholar
- Araújo C, Barros CP, Wanke P (2014) Efficiency determinants and capacity issues in Brazilian for-profit hospitals. Health Care Manag Sci 17:126–138. https://doi.org/10.1007/s10729-013-9249-8ArticleGoogle Scholar
- Barnum DT, Walton SM, Shields KL, Schumock GT (2011) Measuring hospital efficiency with Data Envelopment Analysis: nonsubstitutable vs. substitutable inputs and outputs. J Med Syst 35:1393–401. https://doi.org/10.1007/s10916-009-9416-0
- Simar L, Wilson PW (1998) Sensitivity Analysis of Efficiency Scores: How to Bootstrap in Nonparametric Frontier Models. Manage Sci 44:49–61 ArticleGoogle Scholar
- Karagiannis R (2015) A system-of-equations two-stage DEA approach for explaining capacity utilization and technical efficiency. Ann Oper Res 227:25–43. https://doi.org/10.1007/s10479-013-1367-7ArticleGoogle Scholar
- Li H, Dong S, Liu T (2014) Relative efficiency and productivity: a preliminary exploration of public hospitals in Beijing China. BMC Health Services Res 14:158. https://doi.org/10.1186/1472-6963-14-158ArticleGoogle Scholar
- Xu G-C, Zheng J, Zhou Z-J, Zhou C-K, Zhao Y (2015) Comparative Study of Three Commonly Used Methods for Hospital Efficiency Analysis in Beijing Tertiary Public Hospitals China. Chin Med J (Engl) 128:3185–3190. https://doi.org/10.4103/0366-6999.170279ArticleGoogle Scholar
- Gavurova B, Kocisova K (2020) The efficiency of hospitals: platform for sustainable health care system. Entrepreneur Sustain Issues 8:133–146 ArticleGoogle Scholar
- Simar L, Wilson PW (2007) Estimation and inference in two-stage, semi-parametric models of production processes. J Econometr 136:31–64. https://doi.org/10.1016/j.jeconom.2005.07.009ArticleGoogle Scholar
- Mujasi PN, Asbu EZ, Puig-Junoy J (2016) How efficient are referral hospitals in Uganda? A data envelopment analysis and tobit regression approach. BMC Health Serv Res 16:230. https://doi.org/10.1186/s12913-016-1472-9ArticleGoogle Scholar
- Hunt DJ, Link CR (2020) Better outcomes at lower costs? The effect of public health expenditures on hospital efficiency. Appl Econ 52:400–414. https://doi.org/10.1080/00036846.2019.1646405ArticleGoogle Scholar
- García-Cornejo B, Pérez-Méndez JA (2020) Influence of cost systems on efficiency. An analysis of Spanish hospitals using public national databases. Revista de Contabilidad 23:249–62. https://doi.org/10.6018/rcsar.365031
- Fragkiadakis G, Doumpos M, Zopounidis C, Germain C (2016) Operational and economic efficiency analysis of public hospitals in Greece. Ann Oper Res 247:787–806. https://doi.org/10.1007/s10479-014-1710-7ArticleGoogle Scholar
- Wang M-L, Fang H-Q, Tao H-B, Cheng Z-H, Lin X-J, Cai M et al (2017) Bootstrapping data envelopment analysis of efficiency and productivity of county public hospitals in Eastern, Central, and Western China after the public hospital reform. J Huazhong Univ Sci Technolog Med Sci 37:681–692. https://doi.org/10.1007/s11596-017-1789-6ArticleGoogle Scholar
- Ferreira DC, Nunes AM, Marques RC (2020) Operational efficiency vs clinical safety, care appropriateness, timeliness, and access to health care. J Prod Anal 53:355–375. https://doi.org/10.1007/s11123-020-00578-6ArticleGoogle Scholar
- Cinaroglu S (2021) Changes in hospital efficiency and size: An integrated propensity score matching with data envelopment analysis. Socioecon Plann Sci 76:100960. https://doi.org/10.1016/j.seps.2020.100960ArticleGoogle Scholar
- Guillon M, Audibert M, Mathonnat J (2022) Efficiency of district hospitals in Zimbabwe: Assessment, drivers and policy implications. Health Plann Manage 37:271–280. https://doi.org/10.1002/hpm.3337ArticleGoogle Scholar
- Vrabková I, Vaňková I (2021) Efficiency of Human Resources in Public Hospitals: An Example from the Czech Republic. Int J Environ Res Public Health 18:4711. https://doi.org/10.3390/ijerph18094711ArticleGoogle Scholar
- Sommersguter-Reichmann M, Stepan A (2015) The interplay between regulation and efficiency: Evidence from the Austrian hospital inpatient sector. Socioecon Plann Sci 52:10–21. https://doi.org/10.1016/j.seps.2015.09.001ArticleGoogle Scholar
- Wilson A, Kerr B, Bastian N, Fulton L (2012) Financial performance monitoring of the technical efficiency of critical access hospitals: A data envelopment analysis and logistic regression modeling approach. J Healthc Manag /Am Coll Healthc Exec 57:200–12; discussion 212. https://doi.org/10.1097/00115514-201205000-00010
- Banker RD, Chang H (2006) The super-efficiency procedure for outlier identification, not for ranking efficient units. Eur J Oper Res 175:1311–1320. https://doi.org/10.1016/j.ejor.2005.06.028ArticleGoogle Scholar
- Du J, Wang J, Chen Y, Chou S-Y, Zhu J (2014) Incorporating health outcomes in Pennsylvania hospital efficiency: an additive super-efficiency DEA approach. Ann Oper Res 221:161–172. https://doi.org/10.1007/s10479-011-0838-yArticleGoogle Scholar
- Charnes A, Clark CT, Cooper WW, Golany B (1984) A developmental study of data envelopment analysis in measuring the efficiency of maintenance units in the U.S. air forces. Ann Oper Res 2:95–112. https://doi.org/10.1007/BF01874734
- Dyson RG, Allen R, Camanho AS, Podinovski VV, Sarrico CS, Shale EA (2001) Pitfalls and protocols in DEA. Eur J Oper Res 132:245–259. https://doi.org/10.1016/S0377-2217(00)00149-1ArticleGoogle Scholar
- Gannon B (2005) Testing for variation in technical efficiency of hospitals in Ireland. Economic & Social Review
- Fuentes R, Ferrándiz-Gomis R, Fuster-Garcia B (2019) Efficiency of acute public hospitals in the region of Murcia. Spain J Comp Eff Res 8:929–946. https://doi.org/10.2217/cer-2018-0150ArticleGoogle Scholar
- Jain V, Kumar A, Kumar S, Chandra C (2015) Weight restrictions in Data Envelopment Analysis: A comprehensive Genetic Algorithm based approach for incorporating value judgments. Expert Syst Appl 42:1503–1512. https://doi.org/10.1016/j.eswa.2014.09.034ArticleGoogle Scholar
- Dyson RG, Thanassoulis E (1988) Reducing Weight Flexibility in Data Envelopment Analysis. J Oper Res Soc 39:563–576. https://doi.org/10.1057/jors.1988.96ArticleGoogle Scholar
- Charnes A, Cooper WW, Huang ZM, Sun DB (1990) Polyhedral Cone-Ratio DEA Models with an illustrative application to large commercial banks. J Econometr 46:73–91. https://doi.org/10.1016/0304-4076(90)90048-XArticleGoogle Scholar
- Thompson RG, Singleton FD, Thrall RM, Smith BA (1986) Comparative Site Evaluations for Locating a High-Energy Physics Lab in Texas. Interfaces 16:35–49. https://doi.org/10.1287/inte.16.6.35ArticleGoogle Scholar
- Thanassoulis E, Portela MC, Allen R (2004) Incorporating value judgments in DEA. In: Cooper WW, Seiford LM, Zhu J (eds). Handbook on Data Envelopment Analysis, Boston, MA: Springer US; p. 99–138. https://doi.org/10.1007/1-4020-7798-X_4
- Al-Shammari M (1999) A multi-criteria data envelopment analysis model for measuring the productive efficiency of hospitals. Int J Oper Prod Manag 19:879–891. https://doi.org/10.1108/01443579910280205ArticleGoogle Scholar
- Rouyendegh BD, Oztekin A, Ekong J, Dag A (2019) Measuring the efficiency of hospitals: a fully-ranking DEA–FAHP approach. Ann Oper Res 278:361–378. https://doi.org/10.1007/s10479-016-2330-1ArticleGoogle Scholar
- Wei C-K, Chen L-C, Li R-K, Tsai C-H (2011) Using the DEA-R model in the hospital industry to study the pseudo-inefficiency problem. Expert Syst Appl 38:2172–2176. https://doi.org/10.1016/j.eswa.2010.08.003ArticleGoogle Scholar
- Wei C-K, Chen L-C, Li R-K, Tsai C-H, Huang H-L (2012) A study of optimal weights of Data Envelopment Analysis – Development of a context-dependent DEA-R model. Expert Syst Appl 39:4599–4608. https://doi.org/10.1016/j.eswa.2011.10.001ArticleGoogle Scholar
- Ehreth JL (1994) The development and evaluation of hospital performance measures for policy analysis. Med Care 32:568–587. https://doi.org/10.1097/00005650-199406000-00003ArticleGoogle Scholar
- Flokou A, Aletras V, Niakas D (2017) A window-DEA based efficiency evaluation of the public hospital sector in Greece during the 5-year economic crisis. PLoS ONE 12:e0177946. https://doi.org/10.1371/journal.pone.0177946ArticleGoogle Scholar
- Jia T, Yuan H (2017) The application of DEA (Data Envelopment Analysis) window analysis in the assessment of influence on operational efficiencies after the establishment of branched hospitals. BMC Health Serv Res 17:265. https://doi.org/10.1186/s12913-017-2203-6ArticleGoogle Scholar
- Ozcan YA, McCue MJ (1996) Development of a Financial Performance Index for Hospitals: DEA Approach. J Oper Res Soc 47:18–26. https://doi.org/10.1057/jors.1996.2ArticleGoogle Scholar
- Ozcan YA, Luke RD (1993) A national study of the efficiency of hospitals in urban markets. Health Serv Res 27:719–739 Google Scholar
- Lynch JR, Ozcan YA (1994) Hospital closure: an efficiency analysis. Hosp Health Serv Adm 39:205–220 Google Scholar
- Holvad T, Hougaard JL (1993) Measuring technical input efficiency for similar production units: 80 Danish Hospitals. European University Institute
- Valdmanis V, Kumanarayake L, Lertiendumrong J (2004) Capacity in Thai Public Hospitals and the Production of Care for Poor and Nonpoor Patients. Health Serv Res 39:2117–2134. https://doi.org/10.1111/j.1475-6773.2004.00335.xArticleGoogle Scholar
- Färe R, Karagiannis G (2022) Aggregating farrell efficiencies without value data: The case of hospitals. Socio-Economic Planning Sciences 101393. https://doi.org/10.1016/j.seps.2022.101393
- Valdmanis V, Bernet P, Moises J (2010) Hospital capacity, capability, and emergency preparedness. Eur J Oper Res 207:1628–1634. https://doi.org/10.1016/j.ejor.2010.06.018ArticleGoogle Scholar
- Aksezer ÇS (2016) A nonparametric approach for optimal reliability allocation in health services. Intl J Qual Reliab Manage 33:284–294. https://doi.org/10.1108/IJQRM-11-2014-0174ArticleGoogle Scholar
- Villalobos-Cid M, Chacón M, Zitko P, Instroza-Ponta M (2016) A New Strategy to Evaluate Technical Efficiency in Hospitals Using Homogeneous Groups of Casemix : How to Evaluate When There is Not DRGs? J Med Syst 40:103. https://doi.org/10.1007/s10916-016-0458-9ArticleGoogle Scholar
- Chen S, Wu Y, Chen Y, Zhu H, Wang Z, Feng D et al (2016) Analysis of operation performance of general hospitals in Shenzhen, China: a super-efficiency data envelopment analysis. The Lancet 388:S57. https://doi.org/10.1016/S0140-6736(16)31984-5ArticleGoogle Scholar
- Kaya Samut P, Cafrı R (2016) Analysis of the Efficiency Determinants of Health Systems in OECD Countries by DEA and Panel Tobit. Soc Indic Res 129:113–132. https://doi.org/10.1007/s11205-015-1094-3ArticleGoogle Scholar
- Portela MCAS, Camanho AS, Almeida DQ, Lopes L, Silva SN, Castro R (2016) Benchmarking hospitals through a web based platform. Benchmarking: An Intl J ;23:722–39. https://doi.org/10.1108/BIJ-07-2014-0067
- Papadaki Š, Staňková P (2016) Comparison of horizontally integrated hospitals in private and public sectors of czech republic. Econ Sociol 9:180–94. https://doi.org/10.14254/2071-789X.2016/9-3/16
- Du J, Huo J, Zhu J (2016) Data Envelopment Analysis with Output-Bounded Data. Asia Pac J Oper Res 33:1650050. https://doi.org/10.1142/S0217595916500500ArticleGoogle Scholar
- Stankova P, Papadaki Š (2017) A comparison of efficiency of hospitals in the individual regions of the Czech Republic. Scientific Papers of the University of Pardubice, Series D: Faculty of Economics and Administration 24:200–210 Google Scholar
- Arfa C, Leleu H, Goaïed M, van Mosseveld C (2017) Measuring the capacity utilization of public district hospitals in tunisia: Using dual data envelopment analysis approach. Int J Health Policy Manag 6:9–18. https://doi.org/10.15171/ijhpm.2016.66
- Jahangoshai Rezaee M, Yousefi S, Hayati J (2018) A decision system using fuzzy cognitive map and multi-group data envelopment analysis to estimate hospitals’ outputs level. Neural Comput & Applic 29:761–777. https://doi.org/10.1007/s00521-016-2478-2ArticleGoogle Scholar
- Sultan WIM, Crispim J (2018) Are public hospitals reforming efficiently in West Bank? Confl Heal 12:44. https://doi.org/10.1186/s13031-018-0180-yArticleGoogle Scholar
- Mousa W, Aldehayyat JS (2018) Regional efficiency of healthcare services in Saudi Arabia. Middle East Dev J 10:152–174. https://doi.org/10.1080/17938120.2018.1443607ArticleGoogle Scholar
- Kočišová K, Hass-Symotiuk M, Kludacz-Alessandri M (2018) Use of the DEA method to verify the performance model for hospitals. E+M Ekonomie a Management 21:125–40. https://doi.org/10.15240/tul/001/2018-4-009
- Ghiyasi M (2019) A DEA production technology and its usage for incorporation of collaboration in efficiency analysis: an axiomatic approach. Int Trans Oper Res 26:1118–1134. https://doi.org/10.1111/itor.12325ArticleGoogle Scholar
- Li Y, Lei X, Morton A (2019) Performance evaluation of nonhomogeneous hospitals: the case of Hong Kong hospitals. Health Care Manag Sci 22:215–228. https://doi.org/10.1007/s10729-018-9433-yArticleGoogle Scholar
- Babalola TK, Moodley I (2019) Protocol for Investigating the Technical Efficiency of District Hospitals in the Public Health Sector of KwaZulu-Natal. South Africa JMIR Res Protoc 8:e12037. https://doi.org/10.2196/12037ArticleGoogle Scholar
- Ferreira DC, Nunes AM (2019) Technical efficiency of Portuguese public hospitals: A comparative analysis across the five regions of Portugal. Int J Health Plann Manage 34:e411–e422. https://doi.org/10.1002/hpm.2658ArticleGoogle Scholar
- Karahan M (2019) Using data envelopment analysis to measure the technical efficiency of public hospitals in turkey. Ege Akademik Bakis (Ege Academic Review) 19:373–87. https://doi.org/10.21121/eab.475514
- Küçük A, Özsoy VS, Balkan D (2020) Assessment of technical efficiency of public hospitals in Turkey. Eur J Pub Health 30:230–235. https://doi.org/10.1093/eurpub/ckz143ArticleGoogle Scholar
- Manavgat G, Demi̇rci̇ A (2020) Decentralization matter of healthcare and effect on regional healthcare efficiency: Evidence from Turkey. Sosyoekonomi 261–81. https://doi.org/10.17233/sosyoekonomi.2020.02.12
- Li Q, Tian L, Jing X, Chen X, Li J, Chen H (2020) Efficiency and scale effect of county public hospitals in Shandong Province, China: a cross-sectional study. BMJ Open 10:e035703. https://doi.org/10.1136/bmjopen-2019-035703ArticleGoogle Scholar
- Abiodun AJ, Adeyemi KS (2020) Performance role models among public health facilities: An application of data envelopment analysis. Intl J Healthcare Manage 13:193–200. https://doi.org/10.1080/20479700.2017.1397379ArticleGoogle Scholar
- Irwandy, Sjaaf AC, Achadi A, Nadjib M, Ayuningtyas D, Junadi P et al (2020) The efficiency and productivity of public services hospital in indonesia. Enferm Clin 30:236–9. https://doi.org/10.1016/j.enfcli.2020.06.054
- Chitnis A, Mishra DK (2019) Performance Efficiency of Indian Private Hospitals Using Data Envelopment Analysis and Super-efficiency DEA. J Health Manag 21:279–293. https://doi.org/10.1177/0972063419835120ArticleGoogle Scholar
- Cook WD, Harrison J, Imanirad R, Rouse P, Zhu J (2013) Data Envelopment Analysis with Nonhomogeneous DMUs. Oper Res 61:666–676. https://doi.org/10.1287/opre.2013.1173ArticleGoogle Scholar
- Nistor CS, Ştefănescu CA, Crişan A-R (2017) Performance Through Efficiency in the Public Healthcare System – A DEA Approach in an Emergent Country. Studia Universitatis Babes-Bolyai Oeconomica 62:31–49. https://doi.org/10.1515/subboec-2017-0003ArticleGoogle Scholar
- Ali M, Debela M, Bamud T (2017) Technical efficiency of selected hospitals in Eastern Ethiopia. Health Econ Rev 7:24. https://doi.org/10.1186/s13561-017-0161-7ArticleGoogle Scholar
- Jiang S, Min R, Fang P (2017) The impact of healthcare reform on the efficiency of public county hospitals in China. BMC Health Serv Res 17:838. https://doi.org/10.1186/s12913-017-2780-4ArticleGoogle Scholar
- Zheng W, Sun H, Zhang P, Zhou G, Jin Q, Lu X (2018) A four-stage DEA-based efficiency evaluation of public hospitals in China after the implementation of new medical reforms. PLoS ONE 13:e0203780. https://doi.org/10.1371/journal.pone.0203780ArticleGoogle Scholar
- Cavalieri M, Guccio C, Lisi D, Pignataro G (2018) Does the Extent of per Case Payment System Affect Hospital Efficiency?: Evidence from the Italian NHS. Public Finance Review 46:117–149. https://doi.org/10.1177/1091142116651487ArticleGoogle Scholar
- Sultan WIM, Crispim J (2018) Measuring the efficiency of Palestinian public hospitals during 2010–2015: an application of a two-stage DEA method. BMC Health Serv Res 18:381. https://doi.org/10.1186/s12913-018-3228-1ArticleGoogle Scholar
- Guerrini A, Romano G, Campedelli B, Moggi S, Leardini C (2018) Public vs. private in hospital efficiency: Exploring determinants in a competitive environment. Intl J Public Administr 41:181–9. https://doi.org/10.1080/01900692.2016.1256892
- Gandhi AV, Sharma D (2018) Technical efficiency of private sector hospitals in India using data envelopment analysis. Benchmarking: An Intl J 25:3570–91. https://doi.org/10.1108/BIJ-06-2017-0135.
- Hsiao B, Chen L-H, Wu H-T (2019) Assessing performance of Taiwan hospitals using data envelopment analysis: In view of ownership. Int J Health Plann Manage 34:e602–e616. https://doi.org/10.1002/hpm.2676ArticleGoogle Scholar
- İlgün G, Konca M (2019) Assessment of efficiency levels of training and research hospitals in Turkey and the factors affecting their efficiencies. Health Policy and Technology 8:343–348. https://doi.org/10.1016/j.hlpt.2019.08.008ArticleGoogle Scholar
- Yitbarek K, Adamu A, Tsega G, Siraneh Y, Erchafo B, Yewhalaw D et al (2019) Technical Efficiency of Maternal and Reproductive Health Services in Public Hospitals of Oromia Regional State Ethiopia. Health Serv Insights 12:1178632919837630. https://doi.org/10.1177/1178632919837630ArticleGoogle Scholar
- Ahmed S, Hasan MZ, Laokri S, Jannat Z, Ahmed MW, Dorin F et al (2019) Technical efficiency of public district hospitals in Bangladesh: a data envelopment analysis. Cost Eff Resour Alloc 17:15. https://doi.org/10.1186/s12962-019-0183-6ArticleGoogle Scholar
- Kakemam E, Dargahi H (2019) The Health Sector Evolution Plan and the Technical Efficiency of Public Hospitals in Iran. Iran J Public Health 48:1681–1689 Google Scholar
- Ayiko R, Mujasi PN, Abaliwano J, Turyareeba D, Enyaku R, Anguyo R et al (2020) Levels, trends and determinants of technical efficiency of general hospitals in Uganda: data envelopment analysis and Tobit regression analysis. BMC Health Serv Res 20:916. https://doi.org/10.1186/s12913-020-05746-wArticleGoogle Scholar
- Habib AM, Shahwan TM (2020) Measuring the operational and financial efficiency using a Malmquist data envelopment analysis: a case of Egyptian hospitals. Benchmarking: An International Journal 27:2521–36. https://doi.org/10.1108/BIJ-01-2020-0041
- Top M, Konca M, Sapaz B (2020) Technical efficiency of healthcare systems in African countries: An application based on data envelopment analysis. Health Policy Technol 9:62–68. https://doi.org/10.1016/j.hlpt.2019.11.010ArticleGoogle Scholar
- Jing R, Xu T, Lai X, Mahmoudi E, Fang H (2019) Technical Efficiency of Public and Private Hospitals in Beijing, China: A Comparative Study. Int J Environ Res Public Health 17:82. https://doi.org/10.3390/ijerph17010082ArticleGoogle Scholar
- Chowdhury H, Zelenyuk V (2016) Performance of hospital services in Ontario: DEA with truncated regression approach. Omega 63:111–122. https://doi.org/10.1016/j.omega.2015.10.007ArticleGoogle Scholar
- Ancarani A, Di Mauro C, Gitto S, Mancuso P, Ayach A (2016) Technology acquisition and efficiency in Dubai hospitals. Technol Forecast Soc Chang 113:475–485. https://doi.org/10.1016/j.techfore.2016.07.010ArticleGoogle Scholar
- Ferreira DC, Nunes AM, Marques RC (2018) Doctors, nurses, and the optimal scale size in the Portuguese public hospitals. Health Policy 122:1093–1100. https://doi.org/10.1016/j.healthpol.2018.06.009ArticleGoogle Scholar
- Berger M, Sommersguter-Reichmann M, Czypionka T (2020) Determinants of soft budget constraints: How public debt affects hospital performance in Austria. Soc Sci Med 249:112855. https://doi.org/10.1016/j.socscimed.2020.112855ArticleGoogle Scholar
- Ortega-Díaz MI, Ocaña-Riola R, Pérez-Romero C, Martín-Martín JJ (2020) Multilevel Analysis of the Relationship between Ownership Structure and Technical Efficiency Frontier in the Spanish National Health System Hospitals. Int J Environ Res Public Health 17:5905. https://doi.org/10.3390/ijerph17165905ArticleGoogle Scholar
- Pirani N, Zahiri M, Engali KA, Torabipour A (2018) Hospital Efficiency Measurement Before and After Health Sector Evolution Plan in Southwest of Iran: a DEA-Panel Data Study. Acta Inform Med 26:106–110. https://doi.org/10.5455/aim.2018.26.106-110ArticleGoogle Scholar
- Ho FN, Huang C (2020) The interdependencies of marketing capabilities and operations efficiency in hospitals. J Bus Res 113:337–347. https://doi.org/10.1016/j.jbusres.2019.09.037ArticleGoogle Scholar
- Peng Z, Zhu L, Wan G, Coyte PC (2021) Can integrated care improve the efficiency of hospitals? Research based on 200 Hospitals in China. Cost Eff Resour Alloc 19:61. https://doi.org/10.1186/s12962-021-00314-3ArticleGoogle Scholar
- Sielskas A (2021) Determinants of hospital inefficiency. The case of Polish county hospitals. PLOS ONE 16:e0256267. https://doi.org/10.1371/journal.pone.0256267
- Gao Q, Wang D (2021) Hospital efficiency and equity in health care delivery: A study based in China. Socioecon Plann Sci 76:100964. https://doi.org/10.1016/j.seps.2020.100964ArticleGoogle Scholar
- Han A, Lee K-H (2021) The Impact of Public Reporting Schemes and Market Competition on Hospital Efficiency. Healthcare 9:1031. https://doi.org/10.3390/healthcare9081031ArticleGoogle Scholar
- Nayer MY, Fazaeli AA, Hamidi Y (2022) Hospital efficiency measurement in the west of Iran: data envelopment analysis and econometric approach. Cost Eff Resour Alloc 20:5. https://doi.org/10.1186/s12962-022-00341-8ArticleGoogle Scholar
- Hsieh H-M, Clement DG, Bazzoli GJ (2010) Impacts of market and organizational characteristics on hospital efficiency and uncompensated care. Health Care Manage Rev 35:77–87. https://doi.org/10.1097/HMR.0b013e3181c09956ArticleGoogle Scholar
- Ellegaard O, Wallin JA (2015) The bibliometric analysis of scholarly production: How great is the impact? Scientometrics 105:1809–1831. https://doi.org/10.1007/s11192-015-1645-zArticleGoogle Scholar
- Barth M, Haustein S, Scheidt B (2014) The life sciences in German-Chinese cooperation: an institutional-level co-publication analysis. Scientometrics 98:99–117. https://doi.org/10.1007/s11192-013-1147-9ArticleGoogle Scholar
- Charnes A, Cooper WW, Rhodes E (1978) Measuring the efficiency of decision making units. Eur J Oper Res 2:429–444. https://doi.org/10.1016/0377-2217(78)90138-8ArticleGoogle Scholar
- Cooper WW, Seiford LM, Zhu J (2011) Data envelopment analysis: History, Models, and Interpretations. In: Cooper WW, Seiford LM, Zhu J (eds). Handbook on Data Envelopment Analysis, Boston, MA: Springer US; p. 1–39. https://doi.org/10.1007/978-1-4419-6151-8_1
- Nunamaker TR (1983) Measuring routine nursing service efficiency: a comparison of cost per patient day and data envelopment analysis models. Health Serv Res 18:183–208 Google Scholar
- Zakowska I, Godycki-Cwirko M (2020) Data envelopment analysis applications in primary health care: a systematic review. Fam Pract 37:147–153. https://doi.org/10.1093/fampra/cmz057ArticleGoogle Scholar
- Stefko R, Gavurova B, Kocisova K (2018) Healthcare efficiency assessment using DEA analysis in the Slovak Republic. Health Econ Rev 8:6. https://doi.org/10.1186/s13561-018-0191-9ArticleGoogle Scholar
- Oikonomou N, Tountas Y, Mariolis A, Souliotis K, Athanasakis K, Kyriopoulos J (2016) Measuring the efficiency of the Greek rural primary health care using a restricted DEA model; the case of southern and western Greece. Health Care Manag Sci 19:313–325. https://doi.org/10.1007/s10729-015-9324-4ArticleGoogle Scholar
- Johnes J (2006) Data envelopment analysis and its application to the measurement of efficiency in higher education. Econ Educ Rev 25:273–288. https://doi.org/10.1016/j.econedurev.2005.02.005ArticleGoogle Scholar
- Ruggiero J (2006) Measurement error, education production and data envelopment analysis. Econ Educ Rev 25:327–333. https://doi.org/10.1016/j.econedurev.2005.03.003ArticleGoogle Scholar
- Cooper WW, Seiford LM, Tone K, Zhu J (2007) Some models and measures for evaluating performances with DEA: past accomplishments and future prospects. J Prod Anal 28:151–163. https://doi.org/10.1007/s11123-007-0056-4ArticleGoogle Scholar
- Cook WD, Seiford LM (2009) Data envelopment analysis (DEA) – Thirty years on. Eur J Oper Res 192:1–17. https://doi.org/10.1016/j.ejor.2008.01.032ArticleGoogle Scholar
- Emrouznejad A, Parker BR, Tavares G (2008) Evaluation of research in efficiency and productivity: A survey and analysis of the first 30 years of scholarly literature in DEA. Socioecon Plann Sci 42:151–157. https://doi.org/10.1016/j.seps.2007.07.002ArticleGoogle Scholar
- Panwar A, Olfati M, Pant M, Snasel V (2022) A Review on the 40 Years of Existence of Data Envelopment Analysis Models: Historic Development and Current Trends. Arch Computat Methods Eng 29:5397–5426. https://doi.org/10.1007/s11831-022-09770-3ArticleGoogle Scholar
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
- School of Business Administration, Penn State Harrisburg, 777 West Harrisburg Pike, Middletown, PA, 17057, USA Dinesh R. Pai
- College of Business, Eastern Connecticut State University, 83 Windham St, Willimantic, CT, 06226, USA Fatma Pakdil
- Rochester Institute of Technology, Kate Gleason College of Engineering, Rochester, NY, 14623, USA Nasibeh Azadeh-Fard
- Dinesh R. Pai
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
Corresponding author
Ethics declarations
Declarations
We have no personal, commercial, political, governmental, academic, or financial conflicts of interest.
Ethical approval
This research does not require ethical approval as it relies on secondary data from publicly available sources and does not use any human or animal subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
DEA was first proposed by Charnes, Cooper, and Rhodes (CCR) [391], which is based on constant returns to scale (CRS) technology. To overcome the challenges posed by CRS, Banker, Charnes, and Cooper (BCC) [176] extended the CCR model to incorporating variable returns to scale (VRS) technology assumption. The CCR and BCC models have seen significant development since their inception. The technique is based on the empirical estimation of a frontier through the application of a mathematical programming model to the observed data [12]. This frontier identifies the most efficient combinations of inputs and outputs. Cooper et al. [392] provide an introduction to the basic DEA models and theoretical extensions. Hospital efficiency was the first ranking DEA application in healthcare [6]. Nunamaker [393] was the first to apply DEA in healthcare, whereas Sherman [232] was the first to focus on hospital efficiency applications in the literature. Literature shows that DEA is the most frequently used approach to measure the efficiency of healthcare institutions [25]. A vast number of studies in the hospital efficiency literature use an input-oriented DEA approach [9, 394]. Hospitals, especially community hospitals, cannot choose their output level, which depends on the demand for healthcare services. Furthermore, in a majority of countries, hospital administrators and policymakers generally have more control over input resources compared with outputs. The focus is on controlling costs rather than increasing demand for healthcare (O’Neill et al., 2008). Stefko et al. [395] argue that the aim of hospitals is not to reduce inputs and costs but to focus on increasing outputs by improving the quality of services and patient satisfaction. Oikonomou et al. [396] claim input reduction in the provision of health services is undesirable, while an increase in outputs in many health centers is feasible. Several studies have therefore used an output-oriented approach. Yet, many studies have applied both input- and output-oriented approaches to the same dataset. The choice of orientation, however, depends on the objectives of production units under relevant production and management constraints [262].
DEA brings several advantages to researchers. First, DEA functions with multiple inputs and outputs in mathematical programming. Second, using a benchmarking approach, DEA measures the relative efficiency of the DMUs included in the analysis. Third, DEA gives flexibility to researchers regarding the structure and type of the data, including optimization direction, DMUs, inputs, and outputs. Fourth, because DEA has a non-parametric nature and a mathematical programming structure, it does not include the risk of misspecification of the production function [169]. Finally, the efficiency scores obtained through DEA can be used as a dependent variable in second-stage analyses, usually post hoc regression analyses, to determine the impact of environmental factors on hospital efficiency. DEA, however, has several disadvantages. First, the results are potentially sensitive to the selection of inputs and outputs. Furthermore, the number of efficient firms on the frontier tends to increase with the number of input and output variables. This is one of the reasons we do not compare results from manuscripts reviewed in this study. Second, being a nonparametric technique, DEA does not provide statistical tests of the significance of the input or output variables included in the model [397]. To partially overcome these limitations, prior studies have performed DEA on a variety of specifications to check the sensitivity of the results. Finally, the performance of DEA, an extreme point technique, deteriorates in the presence of measurement error and statistical noise [398]. Since DEA was first developed in 1978, a variety of models and extensions, including hybrid DEA models, have been proposed to mitigate some of its drawbacks and enhance its performance. Each model, though, has both advantages and disadvantages. For a thorough discussion on various models, we recommend the readers refer to Cooper et al. [399], Cook and Seiford [400], and Emrouznejad et al. [401]. Additionally, we refer readers to Panwar et al. [402] for an extensive examination of the advantages and disadvantages of DEA models, including hybrid DEA models.
Appendix 2
Table 2 Distribution of the journals publishing reviewed articles
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pai, D.R., Pakdil, F. & Azadeh-Fard, N. Applications of data envelopment analysis in acute care hospitals: a systematic literature review, 1984–2022. Health Care Manag Sci 27, 284–312 (2024). https://doi.org/10.1007/s10729-024-09669-4
- Received : 01 August 2022
- Accepted : 20 February 2024
- Published : 04 March 2024
- Issue Date : June 2024
- DOI : https://doi.org/10.1007/s10729-024-09669-4
Share this article
Anyone you share the following link with will be able to read this content:
Get shareable link
Sorry, a shareable link is not currently available for this article.
Copy to clipboard
Provided by the Springer Nature SharedIt content-sharing initiative
Keywords
- DEA
- Acute care hospitals
- Systematic literature review